Rhinocort
Laurajo Ryan, PharmD, MSc, BCPS, CDE
- Clinical Associate Professor, Division of Pharmacotherapy, The University of Texas at Austin College of Pharmacy, UT Health Science Center San Antonio, San Antonio, Texashttps://sites.utexas.edu/cpe-hps/speakers-2/ryan/
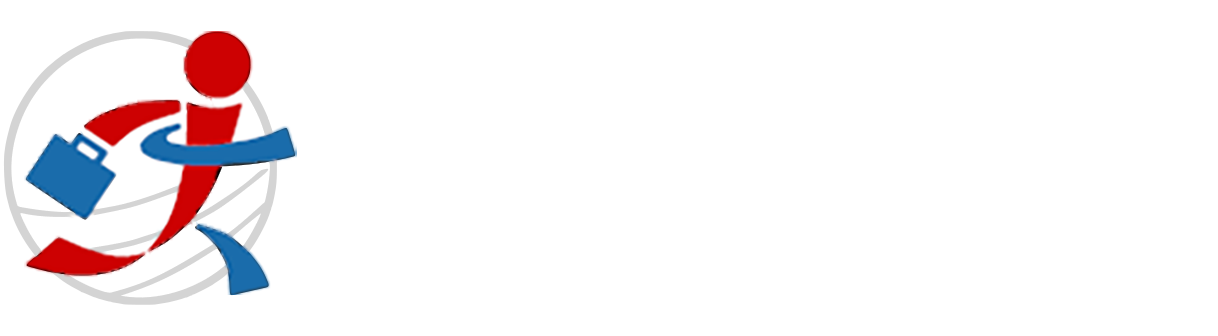
Two or three simple questions can be asked to elicit symptoms of oral dryness allergy shots weight loss purchase rhinocort with a visa, pain or bleeding in the mouth allergy symptoms 8-10 buy discount rhinocort on line, oral hygiene and dietary habits allergy treatment home remedies buy rhinocort 200mcg cheap, and length of time since the patient last saw a dentist allergy treatment otc purchase discount rhinocort. Practices that have not developed these skills among medical assistants may assign providers to conduct the oral exam allergy shots reactions swelling order discount rhinocort on line. Local Workfows Providing fexibility is important allergy treatment systems inc order generic rhinocort canada, particularly while new workfows are being developed and tested. Marshfeld Clinic carefully standardized the oral exam ("Look") process, but gives each care team the fexibility to assign tasks to staff. Some providers conduct the oral exam, while others delegate it to a member of their team, typically a medical assistant. Review information gathered; share results with patients and families; and determine course of action using standardized criteria based on the answers to the screening and risk assessment questions, fndings of the oral exam, and the values, preferences, and goals of the patient and family. Activity 4: Act by delivering preventive interventions and/or placing an order for a referral to a dentist or medical specialist. The provider should also ask for the patient and/or familys permission before making such an introduction. If a care manager or health educator is not available, the primary care practice will need to determine how it can best support these activities. For example, "It is important for you to brush for two minutes, twice a day, concentrating on the gum line, using a fuoride toothpaste. For example, information could be provided in the waiting room or in after-visit summaries. Activity 5: Document the fndings so that the information can be used to provide continuity in patient care, both within the primary care practice and to coordinate care with dentists and medical specialists. Documentation is also essential to measure care processes and monitor clinical outcomes so that quality of care can be managed (Follow Up). They also can document symptoms for such conditions as urinary tract infections and respiratory infections using standardized written protocols. The questions in the "Ask" portion of the Oral Health Delivery Framework likewise may be entered by a medical assistant and the answers reviewed by the clinician. The work of data entry is made easier by designing data entry felds with delimiters that reduce errors by restricting information to a specifc format and expected range of values. We recognize that many primary care practices may not yet have all of the capacities or resources of an advanced primary care practice, and encourage these practices to consider ways they might address oral health, even if implementation of the full Framework is not possible initially. Regardless of where or how a practice begins, the goal is to pursue progressively higher levels of integration, so that over time all patients can expect to receive oral health preventive services and structured referrals from their primary care team. Structured Referrals Many of the patients screened in the course of a primary care visit will meet the criteria for a referral to dentistry, such as those with symptoms or signs of caries or gingivitis. For most practices, this will require developing a network of dentists to which they can refer patients (termed a "primary care-dentistry referral network" in this paper); developing referral agreements similar to those they have with medical specialists, and applying referral support and care coordination processes for referrals to and from dentistry. A "structured" dental referral should include the information the dentist needs to participate appropriately in the patients care, for example: the patients problem list, current medication and allergy lists, the specifc reason for the referral, and a statement that the patient is healthy enough to undergo routine dental procedures. Notifcation that the patient has been scheduled with the dentist (and the date) should be sent to the referring primary care provider; once the patient is seen by the dentist, a summary of the fndings and treatment plan need to be returned to the referring provider so it can be included in the patients health record. Qualis Health | Oral Health: An Essential Component of Primary Care | White Paper 31 Developing a Referral Network Whenever possible, the primary care team should support patients existing relationships by referring patients with a regular source of dental care to their respective dentist. It can be expected, however, that many patients seen in the primary care setting will not yet have a relationship with a dentist and will need guidance. We recommend that primary care practices identify dentists in their community they believe will be open to participating in a primary care-dentistry referral network. If the primary care practice is not aware of dentists in its local area, or needs a broader network to serve its patients, it can contact the local dental society for information. Dental societies may be able to recommend specifc dentists open to new patients or provide a forum for addressing dentists as a group to discuss referral processes and resources. Interested dentists would then be able to ask questions and signal interest in participating in a primary care referral network. Developing primary care-dentistry referral networks will take effort and commitment from primary care providers, dentists, and their respective teams. For these relationships to be successful, dentists should remain open to caring for patients of mixed insurance statuses. Cultivating Referral Relationships Marshfeld Clinic knew that many of its patients did not have dental insurance and would not be able to pay for dental care out of pocket. They were thrilled that doctors considered them part of the health community and respected the role they have. This can be facilitated by an agreement that outlines expectations; for example, the range of clinical indications for referrals, information to accompany a patient, standards for a timeframe in which patients are to be seen, and the information that will be shared with the referring provider. Support needs may include transportation, medical interpretation, or other services. Provider satisfaction is highest when standard formats are used to transmit information between referring providers and consultants. As is the case for medical specialty referrals, it is the primary care teams responsibility to track these key steps. It is the dentists responsibility to communicate information back to the referring primary care provider. Expecting the patient or family to ferry information between the referring provider and consultant, or sharing verbal updates, is not consistent with standards of patient-centered, high-quality care. Expecting the patient or family to ferry information between medical and dental providers is not consistent with standards of patient-centered, high-quality care. Qualis Health | Oral Health: An Essential Component of Primary Care | White Paper 33 Leveraging Health Information Technology Advances in the use of health information technology have resulted in a set of tools that can help primary care teams address their patients oral health needs. These include reporting functionalities, which can assist the care team in conducting risk assessments and tracking results; and after-visit summaries and patient portals, which can make it easier to provide patients and families with relevant and tailored. Figure 5 provides a visual for how information about oral health might can be gathered, used, and shared. These diagnostic entries serve as measurable markers for the "Decide" component of the Oral Health Delivery Framework, with recognition that actual diagnoses may by changed or updated after a dental exam. Outcomes reports Provider Ask Look Qualis Health | Oral Health: An Essential Component of Primary Care | White Paper 34 Education and Training the concepts of prevention, screening, and early intervention to minimize morbidity are foundational to the practice of medicine and nursing, and will be familiar to all members of the primary care team. However, members of the primary care team may not all have received formal education on oral health conditions or risk assessment and screening techniques. Investing in education is an important frst step for any practice interested in providing preventive oral health care. Well-tested oral health clinical training programs exist for primary care providers, and can be used to develop the skills and confdence of the entire primary care team. Qualis Health | Oral Health: An Essential Component of Primary Care | White Paper 35 Quality Improvement: the Importance of Measurement To monitor the effectiveness of an oral health integration effort and understand its impact on patients, families, and the practice as a whole, we recommend that practices track a set of measures similar to those identifed in Table 1. Ideally, these measures are incorporated into the primary care practices existing quality improvement dashboard and presented transparently alongside other clinical quality data for staff, patients, and other stakeholders to see. These practices also have an obligation to address their patients oral health needs as they strive to provide comprehensive, patient-centered, "whole-person" care. Evolution of the Patient-Centered Medical Home Model of Care In 2007, the major primary care medical associations galvanized the feld with a new approach for delivering high-quality, patient-centered, accessible primary healthcare for children, youth, and adults. One defning principle, a "whole-person orientation," set the expectation that primary care assume responsibility for providing for "all of a patients healthcare needs", or take responsibility for appropriately arranging care with other qualifed professionals. Recognition and certifcation programs were also developed in order to validate a practices medical home capacity. Qualis Health | Oral Health: An Essential Component of Primary Care | White Paper 37 the primary care delivery system is in the midst of a transformation, striving to provide more patient-centered and value-oriented care. This evolution provides new resources, and a new responsibility, for addressing oral health as a component of comprehensive, whole-person care. The care team is also equipped to monitor sub-populations of patients at increased risk, including those with chronic diseases, so that complications can be identifed early and treated early. The care team has processes in place to ensure the patient makes it to the appointment with the specialist, and that the information from the consultation returns to the primary care practice and becomes part of the patients health record. For example, medical assistants now frequently perform tests to detect loss of foot sensation in patients with diabetes. Loss of light touch sensation is then followed by an order to a podiatrist signed by the provider. Oral Health: the Next Frontier While patient-centered care has continued to build momentum, the commitment to a "whole-person orientation" has remained for many, only a goal. In 2014, the integration of behavioral health services was recognized through a complementary set of Joint Principles endorsed by several primary care organizations80 and incorporated into state and national medical home recognition and certifcation programs. Qualis Health | Oral Health: An Essential Component of Primary Care | White Paper 38 Overcoming Real and Perceived Barriers to Integration Concern over real and perceived barriers has limited the number of primary care practices incorporating oral health in routine medical care. Specifc recommendations for supporting actions from stakeholders are described in the next section. Time A common concern with the addition of any new healthcare service is lack of time, particularly for providers. The activities included in the Oral Health Delivery Framework are possible to accomplish in a busy primary care practice, so long as the activities are assigned using the principles of "shared care" and effcient workfows are developed to streamline the transfer of information. By using the principles of team-based care and careful workfow planning, primary care teams have been able to incorporate "additional" services in the past, without a signifcant impact on provider time. They had testimony from a provider and a staff member who shared how easy this was to do. Lack of Evidence-Based Guidelines Evidence-based guidelines exist for preventing early childhood caries,61 as do risk assessment instruments,83 treatment protocols, and resources to support caregiver activation and family self-care. We acknowledge that the evidence base for identifying oral health conditions beyond caries in the primary care setting is limited. We encourage primary care teams to contribute to the growing body of evidence on the benefts of incorporating oral health preventive care in routine medical care. Payment Limitations Payment concerns are valid, and we acknowledge they must be addressed. However unfortunate, payment reform typically lags behind delivery system innovations. Recent experience with behavioral health servicesE and lung cancer screeningF demonstrate that suffcient clinical evidence and consumer pressure are effective motivators for changing public and private health beneft programs. Care Coordination Payments to Support Structured Referrals: Increasingly, payers and policymakers are recognizing the value of care coordination, and are paying primary care providers to manage transitions of care. Some state Medicaid programs pay care coordination or care management fees to primary care providers, as do some commercial insurers. While dentists are not currently included on the list of Medicare-recognized specialists, other oral health specialists are included. Future Payment Opportunities the future of primary care payment is not yet clear, but the general shift away from fee-for-service models to value-oriented models (such as Accountable Care Organizations) can be expected to beneft efforts to integrate behavioral health and oral health in primary care. H For an example, refer to: A Guide to Cignas Preventive Health Coverage for Health Care Professionals. Medical practice acts and other regulations that govern which healthcare professionals are allowed to provide (or be paid for) specifc services vary by state. In most states, with appropriate supervision, non-physician members of the care team can perform the activities of the Framework described under "Ask" and "Look. For this to work safely, the clinician must take responsibility for ensuring that medical assistants have written protocols for the clinical tasks they perform, understand them, and carry them out properly. However, if hygienists or dental assistants are available to a practice, it may be possible to provide additional services. To ensure integration, it is important for these professionals to function as full members of the primary care team. This would include participating in team huddles and quality improvement meetings. Further, while dental professionals can offer an important opportunity to expand the bandwidth of the practice to address patients oral health needs, their presence on the care team should not obviate primary care providers or other medical support staff from fully engaging in preventive oral health care. State dental practice acts and other rules and regulations may require non-dentist dental professionals to work under the supervision of a dentist in some states; primary care practices can explore options available to them in their state. Before implementing their integrated oral health program, Confuence Healths Wenatchee Pediatric Clinic asked patients if they would be interested in receiving oral health services in the primary care setting. There dentists and primary care providers working together to are concerns that dentists in some communities may identify children with disease and connect them to care. Strategies to cultivate referral resources for been successful in engaging both dentists in providing uninsured and Medicaid patients follow. Such arrangements are most successful if they are based on personal relationships between medical providers and dentists in the same neighborhood. In addition, some state dental associations maintain lists of free or reduced fee dental practices, which could serve as a referral site for patients without dental insurance.
Prevalence of infective endocarditis in patients diseases consultation lowers mortality from Staphylococcus aureus bactere with Staphylococcus aureus bacteraemia: the value of screening with mia allergy xanax order rhinocort 100 mcg without prescription. Use of a simple criteria set for infectiousdiseasephysiciansandattendingphysicianscanresultinbetter guiding echocardiography in nosocomial Staphylococcus aureus bactere management and outcome for patients with Staphylococcus aureus bac mia allergy symptoms+swollen joints order cheapest rhinocort and rhinocort. Impact of infectious Treatment duration for uncomplicated Staphylococcus aureus bactere disease specialist consultations on outcomes of Staphylococcus aureus mia to prevent relapse: analysis of a prospective observational cohort bacteremia in a hospital with a low volume of patients with S allergy forecast order rhinocort amex. Comparative effectiveness of nafcillin or cefazolin versus vanco cloxacillin with and without gentamicin in short-term therapy for right mycininmethicillin-susceptibleStaphylococcusaureusbacteremia allergy symptoms eyes hurt discount rhinocort 100mcg without a prescription. Menichetti F cat allergy shots uk cost of rhinocort, Martino P allergy treatment naturopathy generic 200 mcg rhinocort with visa, Bucaneve G, Gentile G, DAntonio D, Liso V, aureusindrugabusers. Fortun J, Navas E, Martinez-Beltran J, Perez-Molina J, Martin-Davila InfectionProgram. Short-course therapy for right-side in initial empirical antibiotic regimen for febrile, neutropenic patients endocarditis due to Staphylococcus aureus in drug abusers: cloxacillin with hematologic malignancies. Antimicrob Agents Chemother 38: versus glycopeptides in combination with gentamicin. Raad I, Darouiche R, Vazquez J, Lentnek A, Hachem R, Hanna H, cin in the treatment of Staphylococcus aureus bacteraemia. Persistence in Staphylococcus aureus the 21st century: the International Collaboration on Endocarditis bacteremia: incidence, characteristics of patients and outcome. The role of vancomycin in the persistence or recurrence of Staph Doco-Lecompte T, Celard M, Poyart C, Strady C, Chirouze C, Bes M, ylococcus aureus bacteraemia. Health care exposure and age in infective ment of hemodialysis-dependent patients with methicillin-susceptible endocarditis: results of a contemporary population-based pro le of 1536 Staphylococcus aureus bacteremia. Determinants of the occurrence of and survival from Olaison L, Eykyn S, Hoen B, Abrutyn E, Raoult D, Bayer A, Fowler prosthetic valve endocarditis. Staphylococcus aureus native valve infective endocarditis: erative Study on Valvular Heart Disease. Contemporary clinical pro le and outcome in-hospital death in infective endocarditis. Prognostic value of echocardiography: a prospec Prospective Cohort Study Investigators. Infective endocarditis at a in a series of 122 cases and consequences for treatment decision. Pro leofinfectiveendocarditisatBrazzavilleUniversity endocarditis among patients with prosthetic valves and Staphylococcus Hospital. Infective endocarditis in sub-Saharan African chil thetic valve endocarditis resulting from nosocomial bacteremia. A pro dren, cross-sectional study about 19 cases in Ouagadougou at Burkina spective, multicenter study. Letaief A, Boughzala E, Kaabia N, Ernez S, Abid F, Ben Chaabane T, Sinha B, Herrmann M, Francioli P, Vaudaux P, Moreillon P. Ben Jemaa M, Boujnah R, Chakroun M, Daoud M, Gaha R, Kafsi N, Fibrinogen and bronectin binding cooperate for valve infection and Khalfallah A, Slimane L, Zaouali M. Epidemiology of infective invasion in Staphylococcus aureus experimental endocarditis. Early lessons from the International Collabora of human platelet aggregation by Staphylococcus aureus: roles for the tion on Endocarditis investigation. Endocarditis caused by Staphylococcus aureus:a human-likelow-gradebacteremiamodelofexperimentalendocarditisto reappraisal of the epidemiologic, clinical, and pathologic manifestations study the role of Staphylococcus aureus adhesins and platelet aggregation 640 cmr. Mod factor and bronectin-binding protein by expression in Lactococcus lac i cation of the diagnostic criteria proposed by the Duke Endocarditis tis. Staphylococcus aureus prosthetic valve endocarditis: optimal man genotype and a distinct repertoire of enterotoxins and adhesins. Comparison of Staphylococcus aureus strains for ability to dorsed by the European Society of Clinical Microbiology and Infectious cause infective endocarditis and lethal sepsis in rabbits. Comparison of clinical and morpho Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease logical characteristics of Staphylococcus aureus endocarditis with endo in the Young, Councils on Clinical Cardiology, Stroke, and Cardiovas carditis caused by other pathogens. Methicillin resistant Staphylo microbial therapy, and management of complications. A statement for coccus aureus endocarditis in an Australian tertiary hospital: 1991-2006. Ruotsalainen E, Sammalkorpi K, Laine J, Huotari K, Sarna S, Valtonen Surgery and Anesthesia, American Heart Association: endorsed by the In V, Jarvinen A. Clinical manifestations and outcome in Staphylo fectious Diseases Society of America. Tornos P, Almirante B, Olona M, Permanyer G, Gonzalez T, Carballo treatment of infective endocarditis. Evaluation of daptomycin resistant Staphylococcus aureus with evolving oxacillin susceptibility (the pharmacodynamics and resistance at various dosage regimens against "seesaweffect"). Di Carlo P, DAlessandro N, Guadagnino G, Bonura C, Mammina C, stable small-colony variant in human monocyte-derived macrophages Lunetta M, Novo S, Giarratano A. Dapto monocytes and of daptomycin in combination with gentamicin and/or mycin-nonsusceptible vancomycin-intermediate Staphylococcus aureus rifampin in human monocytes and in broth against Staphylococcus au vertebral osteomyelitis cases complicated by bacteremia treated with reus. High-dose daptomycin prevention of the emergence of daptomycin resistance in Staphylococcus plus fosfomycin is safe and effective in treating methicillin-susceptible and aureus and enterococci following combination with amoxicillin/ methicillin-resistant Staphylococcus aureus endocarditis. High-dose daptomycin and fosfomycin treatment of a patient with experimental model of endocarditis. Additionofgentamicinorrifampindoesnotenhancetheeffective evaluation of the clinical outcomes of daptomycin with and without ness of daptomycin in treatment of experimental endocarditis due to concomitant beta-lactams in patients with Staphylococcus aureus bacte methicillin-resistant Staphylococcus aureus. Susceptibility mycinandnafcillinagainstvancomycin-intermediateStaphylococcusau relationship between vancomycin and daptomycin in Staphylococcus au reus. Beta-lactams increase the antibacterial activity of dap prosthetic valve endocarditis due to Staphylococcus epidermidis. Addition of rifampin to stan coccus aureus in an in vitro model of simulated endocardial vegetations. Initial low-dose gentamicin for Staphylococcus aureus bacteremia gical valve replacement versus medical therapy only. Early surgery in patients with infective endocarditis: a propensity cessfully with antibiotics alone The potential impact of survivor treat methicillin-resistant Staphylococcus aureus in children with no identi ed ment selection bias on the perceived efficacy of valve surgery in the treat predisposing risk. The role of valve surgery in infective endocarditis Staphylococcus aureus in children. Community-acquired methicillin-resistant Staphy D, Delahaye F, Peterson G, Olaison L, Wang A. Dufour P, Gillet Y, Bes M, Lina G, Vandenesch F, Floret D, Etienne J, for treatment-selection bias. What is the optimal methicillin-resistant Staphylococcus aureus skin infections in Southwest timingforsurgeryininfectiveendocarditiswithcerebrovascularcompli ern Alaska. Emergence of community-associated stroke in patients with infective endocarditis may not be safe. Hisata K, Kuwahara-Arai K, Yamanoto M, Ito T, Nakatomi Y, Cui L, endocarditis: the impact of early surgical intervention. High prevalence of methicillin-resistant Staphylo resistantStaphylococcusaureusintheAustraliancommunity:anevolving coccus aureus in emergency department skin and soft tissue infections. PrevalenceanddemographicsofmethicillinresistantStaph ylococcus aureus among professional football players. Staphylococcus aureus among players on a college football team, facili ComparisonofStaphylococcusaureusfromskinandsoft-tissueinfections tated by cosmetic body shaving and turf burns. An epidemic of methicillin-resistant Staphylococcus aureus scriptions for community-onset staphylococcal disease, England. Molecular epidemiology of community ing epidemiology of methicillin-resistant Staphylococcus aureus. Host defense and pathogenesis in of the emergence of community-associated methicillin-resistant Staphy Staphylococcus aureus infections. Cribier B, Prevost G, Couppie P, Finck-Barbancon V, Grosshans E, tissueinfections,andchangesinantibioticchoices,duringtheemergence Piemont Y. Staphylococcus aureus leukocidin: a new virulence fac of community-associated methicillin-resistant Staphylococcus aureus. Epidemiological data on Staphylococcus aureus trends in ambulatory visits and antibiotic prescribing for skin and soft strains producing synergohymenotropic toxins. Widespread skin and soft-tissue infections due to and soft tissue infections as a common cause of hospitalization in United two methicillin-resistant Staphylococcus aureus strains harboring the 644 cmr. Role of antibodies in protection in the Staphylococcus aureus population of Northern Australia. Evolution of virulence in epi munity-associated methicillin-resistant Staphylococcus aureus strains. Role of resistant and methicillin-susceptible Staphylococcus aureus musculoskel the accessory gene regulator agr in community-associated methicillin etal infections in children. Infective pyomyositis and myositis in children in the era of com F, Lu Y, Otto M. McDonald M, Dougall A, Holt D, Huygens F, Oppedisano F, Giffard work of community hospitals. Telavancin versus vancomycin for the Methicillin-resistant Staphylococcus aureus in community-acquired pyo treatment of complicated skin and skin-structure infections associated derma. Deep sternal wound infections following open heart surgery in trimoxazole versus intramuscular benzathine benzylpenicillin for impe Iceland: a population-based study. Epidemiology and outcomes of community-associated infection following coronary artery bypass graft: prevalence, microbiol methicillin-resistant Staphylococcus aureus infection. Inpatient preseptal cellulitis: experience from a tertiary eye cal utility of blood culture results in the identi cation of postoperative care centre. Necrotizing fasciitis ointment as treatment of impetigo: randomized double-blind multicen caused by community-associated methicillin-resistant Staphylococcus tre placebo-controlled trial. Necrotizing cefdinir versus cephalexin for treatment of skin infections in pediatric fasciitis in a medical center in northern Taiwan: emergence of methicil patients. Randomized controlled trial of trimethoprim-sulfamethoxazole for rial skin and skin structure infections. A randomized, cephalexinalonefortreatmentofuncomplicatedcellulitis:arandomized double-blind trial comparing ceftobiprole medocaril with vancomycin controlled trial. Community-onset structure infections: results of 2 double-blind phase 3 comparison stud methicillin-resistant Staphylococcus aureus skin and soft-tissue infec ies with vancomycin-aztreonam. Is Streptococcus pyogenes resistant or complicated skin and skin structure infections caused by Gram-positive susceptible to trimethoprim-sulfamethoxazole Pyogenic vertebral osteomy Giordano P, Lucasti C, Perez A, Good S, Jiang H, Moeck G, ORiordan elitis: analysis of 20 cases and review. Twelve-month out with acute bacterial skin and skin-structure infections: do not let the come following septic arthritis in children. Improved outcome of clinda trends in adult-onset septic arthritis of the knee and hip: retrospective mycin compared with beta-lactam antibiotic treatment for invasive analysis of patients treated during the past 50 years. The microbiology of chronic osteo thetic hip and knee joint infection: treatment and outcomes in Victoria, myelitis: prevalence of resistance to common empirical anti-microbial Australia.
Cheap 200mcg rhinocort overnight delivery. Home Remedies for Fever Coldfever Cough and Cold in Kannada | Kannada Sanjeevani.
Induction of drug tolerance can tine establishment of individual patient drug profiles by some involve IgE immune mechanisms allergy ent best purchase for rhinocort, non-IgE immune mecha hospitals and commercial pharmacies facilitates identification nisms allergy testing negative buy rhinocort cheap, pharmacologic mechanisms allergy symptoms 2013 buy 100 mcg rhinocort mastercard, and undefined mecha of potential allergic reactions allergy medicine prescription order rhinocort 200mcg amex. All procedures to induce drug tolerance the management of drug allergy begins with the suspicion involve administration of incremental doses of the drug allergy testing yuma az discount rhinocort 100 mcg on line. The proce tolerance is to modify an individuals immune response to a dure can be performed via oral allergy hacks purchase rhinocort 200mcg without prescription, intravenous, or subcutaneous given drug to allow treatment with it safely. There are no comparative studies to compare the likelihood of drug allergy, a graded challenge or test dose to safety of different routes of induction of drug tolerance, such the specific drug in question may provide a useful confirma as oral vs intravenous. The resulting state is temporary, and tion that administration of the drug will not result in an its maintenance requires continued administration of the of immediate reaction. Induction of drug tolerance procedures vary cautiously administer a drug to a patient who is unlikely to be with individual drugs, and they are intended for agents that allergic to it when there is no intention to alter the immune induce IgE-mediated reactions and, in some cases, for ana response. Patients who tolerate a example, in penicillin induction of drug tolerance, the initial graded challenge are considered to not be allergic to the drug dose is typically approximately 1/10,000 of the full therapeu and are not at increased risk for future reactions compared tic dose. The use of prophylactic medi previous dose and are administered at 15 to 30-minute in cations to prevent systemic reactions in these procedures is tervals until therapeutic levels are achieved. These protocols require the supervision of a health the procedure varies, depending on the drug and route of care professional with previous experience performing these administration, but, in most cases, can be accomplished procedures. Induction of drug tolerance should be the choice of whether to introduce a clinically indicated performed in an appropriate setting, supervised by physicians drug via graded challenge or via induction of drug tolerance familiar with the procedure, with continual monitoring of the mainly depends on the likelihood that the patient is allergic at patient and readiness to treat reactions, including anaphy the time of the procedure. Induction of drug tolerance protocols and/or diagnostic test results, are unlikely to be allergic to a are available for a variety of drugs, including virtually all drug may undergo graded challenge. For example, if penicil classes of antibiotics, insulin, chemotherapeutic agents, and lin skin testing is unavailable and a patient with a history of biological agents, such as humanized monoclonal antibod a mild pruritic rash during penicillin treatment 30 years ago ies. Patients who have a imately a third of patients who undergo penicillin induction relatively higher likelihood of being allergic to a drug should of drug tolerance experience allergic reactions, which are undergo an induction of drug tolerance procedure. For exam generally mild and occur predominantly after the procedure, ple, if penicillin skin testing is unavailable and a patient with during treatment with penicillin. Example of Intravenous Cephalosporin IgE Induction of Tolerance (eg, Desensitization) Protocol. These are typically performed over hours to days with an initial dose in the milligram range. Vancomycin Induction of Drug Tolerance Procedure344a ceptions, such as when benefit of treatment of a life-threat Concentration Infusion Vancomycin Time, Cumulative of vancomycin, rate, infusion rate, min dose, mg mg/mL mL/min mg/min Table 6. Representative Paclitaxel Immunologic IgE Induction of Drug Tolerance (eg, Desensitization) Protocol. Six-Hour Trimethoprim-Sulfamethoxazole Induction of aspirin is required for patients to remain in a tolerant state. After aspirin desensitization, loss of tolerance desensitization protocols and continue to experience flares of generally returns in 2 to 4 days after discontinuation of their cutaneous condition with exposure to aspirin or cross continuous aspirin therapy. Ten-Day Trimethoprim-Sulfamethoxazole Induction of Drug Tolerance Procedure680a gram amounts. The protocol differs from both IgE and Day Dosage, mg Concentration/tablet Amount non-IgE induction of drug tolerance. It involves a metabolic shift, reduction in urinary leukotriene E4, internalization of 1 0. Continued daily administration of 325 to 650 mg of available as 40/200/5 mL (8/40 mg/mL). After patient completely stabilized, provoking dose can be Document informed consent and advise patient it may take repeated (assuming another 3 hours of observation time), several days to complete (most will take 2 days). Dosing interval may be extended to 3 hours based on individual patient characteristics. Medications for treatment of aspirin-induced reactions Reactions will likely occur with early doses, usually 81mg. Nasal Antihistamine, topical decongestant After patient completely stabilized (but not less than 3 hours Laryngeal Racemic epinephrine nebulization after the last dose), the provoking dose can be repeated. No confirmatory challenge studies could a this recommended protocol is intended to be more practical, using be performed to determine whether the previous reactions doses based on commercially available 81 mg aspirin products and a were causally or coincidentally associated with aspirin. There are no data on safety and efficacy of this reason, it is uncertain whether these patients were truly this protocol. An example of a rapid aspirin challenge desensitization protocol is provided in Table 13. Allopurinol (High-Risk Patients) Induction of Drug Patients With Coronary Artery Disease Requiring Aspirin366 Tolerance Procedurea Timea Aspirin dose, mg Daily dose Concentration/tablet Amount Days 0 0. Summary Statement 69: Some induction of drug tolerance procedures have been described that appear to be successful induce a severe reaction. An example is the procedures (Tables 14 evaluation, are unlikely to be allergic to the given drug. The and 15) used to induce drug tolerance in patients with histo starting dose for a graded challenge is higher than for induc ries of cutaneous reactions to allopurinol. Although largely tion of drug tolerance, and the number of steps in the proce successful, these protocols have been associated with the dure may be 2 or several. It is possible that a "graded subsequent development of significant adverse reactions. For that reason, future admin Summary Statement 70: the objective of a graded chal istrations of the drug should be given cautiously. The inter lenge is to cautiously introduce a drug in patients who are vals between doses are dependent on the type of previous unlikely to be allergic to it. Unlike induction of drug toler reaction, and the entire procedure may take hours or days to ance, it does not modify patients response to a drug. Because parenteral administration of a drug is Graded challenge (also known as test dosing), unlike in more likely to produce severe anaphylaxis than oral admin duction of drug tolerance, does not modify an individuals istration, more caution should be exercised for graded chal immune response to a given drug. The objective of a graded lenge procedures that use a parenteral route of administration. Depending on the reaction history, the first dose often unclassifiable immune characteristics. Penicillin need for penicillin, rapid induction of drug tolerance may be Summary Statement 71: Approximately 10% of patients performed. Patients with recent or con vincing reaction histories should only receive penicillins via lergy. The negative pre Summary Statement 89: the usefulness of in vitro tests for dictive value of penicillin skin testing for immediate reactions penicillin specific IgE is limited by their uncertain predictive approaches 100%, whereas the positive predictive value is value. When evaluated for penicillin nilloate) may miss up to 20% of allergic patients, but data on allergy, up to 90% of these individuals are able to tolerate this are conflicting. There are several explanations ("aged" penicillin) does not spontaneously degrade to form to account for this discrepancy. Penicillin specific IgE anti antigenic determinants and has no role in penicillin skin bodies are known to rapidly wane over time. Alternatively, penicillin are faced with antibiotic choices that may be less effective, skin testing may be performed when treatment with a peni more toxic, or more expensive and may compromise optimal cillin compound is contemplated. In vitro tests (radioallergosorbent test or enzyme broad-spectrum antibiotics and improve use of antibiotic linked immunoassay) are less sensitive and specific compared selections. Penicillin skin testing detects the pres There are few prospective data on the rate of penicillin ence or absence of penicillin specific IgE antibodies, and it is sensitization. Of the minor determinants, reactions involve cutaneous eruptions, and in a large-scale penicillin G is commercially available and should be used for review of adverse skin reactions of the Boston Collaborative skin testing at a concentration of 10,000 U/mL. The other Drug Surveillance Program, the frequency of skin reactions minor determinants (penicilloate and penilloate) are used for was 5. Penicillin G left in solution morbilliform, or urticarial, and it is unclear how many were ("aged" penicillin) does not spontaneously degrade to form IgE dependent. Life-threatening anaphylactic reactions to other minor determinants and therefore cannot be used as a penicillin are of the most concern, and they appear to be rare. The negative In 1968, in a review of published and unpublished reports, the predictive value of penicillin skin testing (using penicilloyl rate of penicillin-induced anaphylaxis was 0. In a study of children and young adults 17,18,396 for serious immediate-type reactions approaches 100%, receiving monthly injections of benzathine penicillin G for an and the positive predictive value (based on limited challenges average of 3. Among healthy military recruits, 2 mercially available in the United States, most allergists per of 9,203 experienced anaphylaxis after prophylactic treat form penicillin skin tests with only penicilloylpolylysine and ment with a single dose of benzathine penicillin (ie, 2. The haptenate proteins after undergoing conversion to reactive clinical significance of these findings is uncertain. This process occurs spontaneously under phys challenges of individuals skin test negative to penicilloyl iologic conditions, whereas most other antibiotics must be 397,399 metabolized enzymatically to produce intermediates capable polylysine and penicillin G have similar reaction rates of binding to host proteins. The penicillin molecule has a core compared with individuals skin test negative to the full set of major and minor penicillin determinants. Under physiologic conditions, based on the available literature, skin testing with penicilloyl the lactam ring opens spontaneously, allowing the carbonyl polylysine and penicillin G appears to have adequate negative group to form an amide linkage with amino groups of lysine predictive value in the evaluation of penicillin allergy. The most important of are applied by the prick/puncture technique, and if these these are penicilloate and penilloate, and they, along with results are negative, intradermal testing should be performed. Penicillin skin testing, using the reagents de plained by the fact that patients with convincing reaction scribed above and proper technique, are safe with only a rare histories lose their sensitivity over time. Of 239 patients with initially negative peni repeat penicillin skin testing is not indicated in patients with cillin skin test results, 6 patients (2. In a previous study, treatment with penicillin appears to be more likely; there among 614 patients without a history of penicillin allergy, 51 fore, repeat penicillin skin testing in this situation may be (8. Arguments in favor of elective penicilloylpolylysine is poor, and, in that situation, elective skin testing include the fact that penicillin skin testing in the penicillin skin testing is not recommended. Also, in remote acute setting when a patient is ill is more difficult to accom areas, clinicians may not have access to an allergist/immu plish in a timely fashion. Consequently, such patients are nologist to perform penicillin skin testing even if appropriate treated with alternate antibiotics,19,374,376,393 many of which, reagents are available. Overuse of broad-spectrum antibiotics is known to history and likelihood of needing treatment with penicillins. Surveys of patient with cillin specific IgE antibodies wane over time, and therefore negative penicillin skin test results (without subsequently patients with recent reactions are more likely to be allergic being challenged with penicillin) found that a large propor than patients with distant reactions. Approximately 50% of tion was not treated with lactam antibiotics because of fear patients with IgE-mediated penicillin allergy lose their sen on either the part of the patient or the treating physician. This study suggests that penicillin specific full dose, assuming no reaction occurs during a brief obser IgE in some patients may indicate sensitization rather than vation period). Patients with distant (longer than 10 Several studies have addressed the issue of resensitization years) or questionable reaction histories (eg. Resensitization after oral treatment challenge, as opposed to induction of drug tolerance proce with penicillin is rare in both pediatric and adult patients, dure. Clinical cutaneous reactions also may be increased in patients who judgment is required to carefully weigh the risks and benefits have an elevated uric acid, are being treated with allopurinol, of either procedure and informed consent (verbal or written) or have chronic lymphocytic leukemia. If the penicillin skin test to skin testing because these assays have unknown predictive result is negative, the patient should be approached as out value, which limits their usefulness. If the penicillin academic settings, the sensitivity of in vitro tests for penicil skin test result is positive, the patient should be given an lin specific IgE was as low as 45% compared with skin alternative antibiotic or undergo induction of drug tolerance testing. Cephalosporins (Figure 2) of an IgE-mediated allergy; however, a negative in vitro test Summary Statement 92: the overall reaction rate to ceph result does not rule out an IgE-mediated allergy. The negative predictive value dotal evidence suggests that allergic reactions to cephalospo of skin testing with native semisynthetic penicillins is un rins are directed at the R-group side chains rather than the known, and there is no consensus regarding the appropriate core lactam portion of the molecule. Most pa cephalosporin, the following approach may be considered: tients will tolerate future administration of penicillin other (1) after ensuring that 2 cephalosporins do not share R-group than ampicillin and amoxicillin. If ampicillin or amoxicillin is side chains, perform a graded challenge with the new ceph administered again, the patient may develop a similar erup alosporin; (2) perform cephalosporin skin testing (with the tion or no reaction at all. It is postulated that many amoxi agent to be used), although such skin testing is not standard cillin/ampicillin-associated delayed maculopapular rashes re ized and the negative predictive value is unknown; or (3) quire the presence of a concurrent viral illness. Skin testing should be performed as described in the Summary Statement 103: If penicillin and cephalosporin penicillin section with a prick/puncture test followed by an skin testing is unavailable, depending on the reaction history, intracutaneous test (if the prick-test reaction is negative in 10 cephalosporins may need to be given via graded challenge or to 15 minutes). A positive ceph ring structure and moderate cross-reactivity has been docu mented in vitro. A negative cephalosporin skin test (using a cephalosporins is infrequent, anaphylactic reactions after ad nonirritating concentration) does not rule out the presence of ministration of cephalosporin have occurred in patients with drug specific IgE antibodies. Therefore, because the negative predictive were given cephalosporins had a reaction rate of approxi value of cephalosporin skin testing is unknown, a cautious 430,437 mately 10% to 20%. The number of steps in the 1980, all penicillin allergic patients who reacted to a cepha graded challenge and the pace of the challenge are deter losporin had been treated with cephalothin or cephaloridine. Graded challenges require may Benzyl penicillin and these cephalosporins share a similar be performed in an outpatient setting, without intravenous side chain, a finding that could account for increased cross access, but with preparedness to treat severe allergic reac reactivity. If the previous history is consis cephalosporins were contaminated with trace amounts of tent with a severe IgE-mediated reaction, induction of drug penicillin. Cephalosporin Administration to Patients With a If patients with a history of allergy to penicillin are not skin tested but given cephalosporins directly, the chance of a History of Penicillin Allergy (Figure 2) reaction is probably less than 1%.
Special Issues Vaccines the vaccination status of workers should be considered in a risk assessment for workers with this organism and/or toxin allergy medicine safe for pregnancy purchase generic rhinocort. While the risk of laboratory-associated tetanus is low allergy testing yuma discount 100mcg rhinocort overnight delivery, the administration of an adult diphtheria tetanus toxoid at 10-year intervals further reduces the risk to laboratory and animal care personnel of toxin exposures and wound contamination allergy medicine generic name purchase rhinocort with mastercard, and is therefore highly recommended allergy forecast lancaster pa discount 200mcg rhinocort with amex. Corynebacterium diphtheriae Corynebacterium diphtheriae is a pleomorphic gram-positive rod that is isolated from the nasopharynx and skin of humans allergy treatment in toddlers purchase 100 mcg rhinocort otc. The organism is easily grown in the laboratory on media containing 5% sheep blood allergy medicine gsk order rhinocort discount. Natural Modes of Infection the agent may be present in exudates or secretions of the nose, throat (tonsil), pharynx, larynx, wounds, in blood, and on the skin. Travel to endemic areas or close contact with persons who have returned recently from such areas, increases risk. Naturally occurring diphtheria is characterized by the development of grayish white membranous lesions involving the tonsils, pharynx, larynx, or nasal mucosa. An effective vaccine has been developed for diphtheria and this disease has become a rarity in countries with vaccination programs. Francisella tularensis Francisella tularensis is a small gram-negative coccobacillus that is carried in numerous animal species, especially rabbits, and is the causal agent of tularemia (Rabbit fever, Deer fy fever, Ohara disease, or Francis disease) in humans. Type A and Type B strains are highly infectious, requiring only 10-50 organisms to cause disease. The incubation period varies with the virulence of the strain, dose and route of introduction but ranges from 1-4 days with most cases exhibiting symptoms in 3-5 days. Occasional cases were linked to work with naturally or experimentally infected animals or their ectoparasites. Natural Modes of Infection Tick bites, handling or ingesting infectious animal tissues or fuids, ingestion of contaminated water or food and inhalation of infective aerosols are the primary transmission modes in nature. Occasionally, infections have occurred from bites or scratches by carnivores with contaminated mouthparts or claws. Direct contact of skin or mucous membranes with infectious materials, accidental parenteral inoculation, ingestion, and exposure to aerosols and infectious droplets has resulted in infection. Infection has been more commonly associated with cultures than with clinical materials and infected animals. Laboratory personnel should be informed of the possibility of tularemia as a differential diagnosis when samples are submitted for diagnostic tests. Helicobacter species Helicobacters are spiral or curved gram-negative rods isolated from gastrointestinal and hepatobiliary tracts of mammals and birds. There are currently 20 recognized species, including at least nine isolated from humans. Since its discovery in 1982, Helicobacter pylori has received increasing attention as an agent of gastritis. Natural Modes of Infection Chronic gastritis and duodenal ulcers are associated with H. Transmission, while incompletely understood, is thought to be by the fecal-oral or oral-oral route. Legionella pneumophila and other Legionella-like Agents Legionella are small, faintly staining gram-negative bacteria. They are obligately aerobic, slow-growing, nonfermentative organisms that have a unique requirement for L-cysteine and iron salts for in vitro growth. There are currently 48 known Legionella species, 20 of which have been associated with human disease. Natural Modes of Infection Legionella is commonly found in environmental sources, typically in man-made warm water systems. The mode of transmission from these reservoirs is aerosolization, aspiration or direct inoculation into the airway. The spectrum of illness caused by Legionella species ranges from a mild, self-limited fu-like illness (Pontiac fever) to a disseminated and often fatal disease characterized by pneumonia and respiratory failure (Legionnaires disease). Although rare, Legionella has been implicated in cases of sinusitis, cellulitis, pericarditis, and endocarditis. Surgery, especially involving transplantation, has been implicated as a risk factor for nosocomial transmission. Laboratory Safety and Containment Recommendations the agent may be present in respiratory tract specimens (sputum, pleural fuid, bronchoscopy specimens, lung tissue), and in extrapulmonary sites. A potential hazard may exist for generation of aerosols containing high concentrations of the agent. Leptospira the genus Leptospira is composed of spiral-shaped bacteria with hooked ends. Leptospires are ubiquitous in nature, either free-living in fresh water or associated with renal infection in animals. These organisms also have been characterized serologically, with more than 200 pathogenic and 60 saprophytic serovars identifed as of 2003. Growth of leptospires in the laboratory requires specialized media and culture techniques, and cases of leptospirosis are usually diagnosed by serology. Animals with chronic renal infection shed large numbers of leptospires in the urine continuously or intermittently, for long periods of time. Common routes of infection include abrasions, cuts in the skin or via the conjunctiva. Higher rates of infection observed in agricultural workers and other occupations associated with animal contact. Laboratory Safety and Containment Recommendations the organism may be present in urine, blood, and tissues of infected animals and humans. Ingestion, accidental parenteral inoculation, and direct and indirect contact of skin or mucous membranes, particularly the conjunctiva, with cultures or infected tissues or body fuids are the primary laboratory hazards. Gloves should be worn to handle and necropsy infected animals and to handle infectious materials and cultures in the laboratory. Listeria monocytogenes Listeria monocytogenes is a gram-positive, non-spore-forming, aerobic bacillus; that is weakly beta-hemolytic on sheep blood agar and catalase-positive. It may also be isolated from symptomatic/asymptomatic animals (particularly ruminants) and humans. Occupational Infections Cutaneous listeriosis, characterized by pustular or papular lesions on the arms and hands, has been described in veterinarians and farmers. In pregnant women, Listeria monocytogenes infections occur most often in the third trimester and may precipitate labor. While ingestion is the most common route of exposure, Listeria can also cause eye and skin infections following direct contact with the organism. Gloves and eye protection should be worn while handling infected or potentially infected materials. Due to potential risks to the fetus, pregnant women should be advised of the risk of exposure to L. Mycobacterium leprae Mycobacterium leprae is the causative agent of leprosy (Hansen disease). The organism has not been cultivated in laboratory medium but can be maintained in a metabolically active state for some period. Organisms are recovered from infected tissue and can be propagated in laboratory animals, specifcally armadillos and the footpads of mice. Occupational Infections There are no cases reported as a result of working in a laboratory with biopsy or other clinical materials of human or animal origin. However, inadvertent human-to human transmissions following an accidental needle stick by a surgeon and after use of a presumably contaminated tattoo needle were reported prior to 1950. Laboratory Safety and Containment Recommendations the infectious agent may be present in tissues and exudates from lesions of infected humans and experimentally or naturally infected animals. Direct contact of the skin and mucous membranes with infectious materials and accidental parenteral 144 Biosafety in Microbiological and Biomedical Laboratories inoculation are the primary laboratory hazards associated with handling infectious clinical materials. Extraordinary care should be taken to avoid accidental parenteral inoculation with contaminated sharp instruments. Mycobacterium tuberculosis complex the Mycobacterium tuberculosis complex includes M. The organism has a thick, lipid-rich cell wall that renders bacilli resistant to harsh treatments including alkali and detergents and allows them to stain acid-fast. The primary focus of infection is the lungs, but most other organs can be involved. It is spread to humans, primarily children, by consumption of non pasteurized milk and milk products, by handling of infected carcasses, and by inhalation. Exposure to laboratory-generated aerosols is the most important hazard encountered. Tubercle bacilli may survive in heat-fxed smears108 and may be aerosolized in the preparation of frozen sections and during manipulation of liquid cultures. Use of a slide-warming tray, rather than a fame, is recommended for fxation of slides. However, considerable care must be exercised to verify the identity of the strain and to ensure that cultures are not contaminated with virulent M. Many of the species are common environmental organisms, and approximately 25 of them are associated with infections in humans. All of these species are considered opportunistic pathogens in humans and none are considered communicable. Mycobacteria are frequently isolated from clinical samples but may not be associated with disease. Agent Summary Statements: Bacterial Agents 147 Occupational Infections Laboratory-acquired infections with Mycobacterium spp. Natural Modes of Infection Person-to-person transmission has not been demonstrated. Presumably, pulmonary infections are the result of inhalation of aerosolized bacilli, most likely from the surface of contaminated water. They are also common in potable water supplies, perhaps as the result of the formation of bioflms. Laboratory Safety and Containment Recommendations Various species of mycobacteria may be present in sputa, exudates from lesions, tissues, and in environmental samples. Direct contact of skin or mucous membranes with infectious materials, ingestion, and accidental parenteral inoculation are the primary laboratory hazards associated with clinical materials and cultures. Aerosols created during the manipulation of broth cultures or tissue homogenates of these organisms also pose a potential infection hazard. Selection of an appropriate tuberculocidal disinfectant is an important consideration for laboratories working with mycobacteria. Neisseria gonorrhoeae Neisseria gonorrhoeae is a gram-negative, oxidase-positive diplococcus associated with gonorrhea, a sexually transmitted disease of humans. The organism may be isolated from clinical specimens and cultivated in the laboratory using specialized growth media. Natural Modes of Infection Gonorrhea is a sexually transmitted disease of worldwide importance. The 2004 rate of reported infections for this disease in the United States was 112 per 100,000 population. This usually occurs by sexual activity, although newborns may also become infected during birth. Accidental parenteral inoculation and direct or indirect contact of mucous membranes with infectious clinical materials are known primary laboratory hazards. Gloves should be worn when handling infected laboratory animals and when there is the likelihood of direct skin contact with infectious materials. Neisseria meningitidis Neisseria meningitidis is a gram-negative coccus responsible for serious acute meningitis and septicemia in humans. Thirteen different capsular serotypes have been identifed, with types A, B, C, Y, and W135 associated with the highest incidence Agent Summary Statements: Bacterial Agents 149 of disease. Almost all the microbiologists had manipulated sterile site isolates on an open laboratory bench. Natural Modes of Infection the human upper respiratory tract is the natural reservoir for N. Invasion of organisms from the respiratory mucosa into the circulatory system causes infection that can range in severity from subclinical to fulminant fatal disease. Transmission is person-to-person and is usually mediated by direct contact with respiratory droplets from infected individuals. Parenteral inoculation, droplet exposure of mucous membranes, infectious aerosol and ingestion are the primary hazards to laboratory personnel. Based on the mechanism of natural infection and the risk associated with handling of isolates on an open laboratory bench, exposure to droplets or aerosols of N. Special Issues Vaccines the quadrivalent meningococcal polysaccharide vaccine, which includes serogroups A, C, Y, and W-135, will decrease but not eliminate the risk of infection, because it is less than 100% effective and does not provide protection against serogroup B, which caused one-half of the laboratory-acquired cases in the United States in 2000. Typhi Salmonellae are gram-negative enteric bacteria associated with diarrheal illness in humans. They are motile oxidase-negative organisms that are easily cultivated on standard bacteriologic media, although enrichment and selective media may be required for isolation from clinical materials. Occupational Infections Salmonellosis is a documented hazard to laboratory personnel. Case reports of laboratory-acquired infections indicate a presentation of symptoms (fever, severe diarrhea, abdominal cramping) similar to those of naturally-acquired infections, although one case also developed erythema nodosum and reactive arthritis. An estimated 5 million cases of salmonellosis occur annually in the United States. A wide range of domestic and feral animals (poultry, swine, rodents, cattle, iguanas, turtles, Agent Summary Statements: Bacterial Agents 151 chicks, dogs, cats) may serve as reservoirs for this disease, as well as humans. The disease usually presents as an acute enterocolitis, with an incubation period ranging from 6 to 72 hours. Laboratory Safety and Containment Recommendations the agent may be present in feces, blood, urine, and in food, feed, and environmental materials.