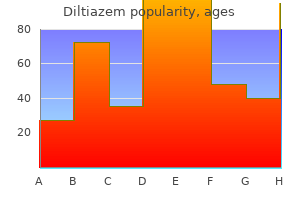
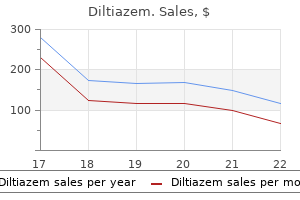
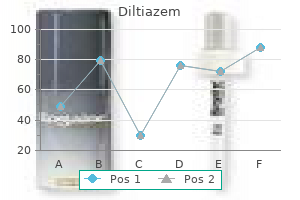
Diltiazem
Jessica H. Brady, PharmD, BCPS
- Clinical Associate Professor, Department of Clinical Sciences, School of Pharmacy, University of Louisiana at Monroe
- Adult Medicine Clinical Pharmacist, University Health Conway, Monroe, Louisiana
https://www.linkedin.com/in/jessica-brady-b43237113
Restrictive versus liberal blood transfusion policy for hepatectomies in cirrhotic patients medications post mi buy 180mg diltiazem overnight delivery. Can hepatic failure after surgery for hepatocellular carcinoma in cirrhotic patients be prevented Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure medicine 81 buy generic diltiazem online. Morbidity and mortality after major hepatic resection in cirrhotic patients with hepatocellular carcinoma symptoms 24 purchase diltiazem 60mg line. Perioperative nutritional support Surgical management of hepatobiliary and pancreatic disorders 122 in patients undergoing hepatectomy for hepatocellular carcinoma symptoms 7 days after implantation order diltiazem. Effect of enteral nutrition on the short outcome of severely malnourished cirrhotics symptoms for bronchitis discount diltiazem 60 mg free shipping. Hepatectomies pour hepatocarcinome sur foie cirrhotique: schemas decisionnels et principes de reanimation peri-operatoire symptoms nerve damage diltiazem 60 mg. Prognostic factors of hepatocellular carcinoma in patients undergoing hepatic resection. Hepatic resection of hepatocellular carcinoma in cirrhotic liver: is it unjustified in impaired liver function Monoethylglycinexylidide formation measurement as a hepatic function test to assess severity of chronic liver disease. Liver resection in the aged (seventy years or older) with hepatocellular carcinoma. Hepatocellular carcinoma in the elderly: results of surgical and nonsurgical management. Results of major liver resection for large hepatocellular carcinoma in patients with cirrhosis. Percutaneous portal vein embolization increases the feasibility and safety of major liver resection for hepatocellular carcinoma in the injured liver. Prolonged normothermic ischaemia of human cirrhotic liver during hepatectomy: a preliminary report. Segmental liver resection using ultrasoundguided selective portal venous occlusion. Patterns of improvement in resection of hepatocellular carcinoma in cirrhotic patients. An isolated, complete resection of the Surgical management of hepatobiliary and pancreatic disorders 124 caudate lobe, including the paracaval portion, for hepatocellular carcinoma. Autologous blood transfusion for hepatectomy in patients with cirrhosis and hepatocellular carcinoma: use of recombinant human erythropoietin. Treatment of small hepatocellular carcinoma in cirrhotic patients: a cohort study comparing surgical resection and percutaneous ethanol injection. No treatment, resection and ethanol injection in hepatocellular carcinoma: a retrospective analysis of survival in 391 patients with cirrhosis. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Liver resection for hepatocellular carcinoma: results of 229 consecutive patients during 11 years. Pattern of recurrence of hepatocellular carcinoma after liver transplantation: Milan multicenter experience. The prediction of risk of recurrence and time to recurrence of hepatocellular carcinoma after orthotopic liver transplantation: a pilot study. Preoperative selective portal vein embolizations are an effective means of extending the indications of major hepatectomy in the normal and injured liver. Primary liver resection and salvage transplantation or primary liver transplantation in patients with single, small hepatocellular carcinoma and preserved liver function: an outcome-orientated decision analysis. The role of transplantation in small hepatocellular carcinoma complicating cirrhosis of the liver. A multidisciplinary approach to hepatocellular carcinoma in patients with cirrhosis. Is hepatocellular carcinoma in cirrhosis an actual indication for liver transplantation Is transplantation really superior to resection in the treatment of small hepatocellular carcinoma David L Bartlett and Yuman Fong Introduction the management of patients with small hepatic metastases from colorectal cancer and other histologies requires the consideration of many diverse patient and tumor related factors. These factors include the natural history of the tumor type, the expected cure rate after surgical treatment, effectiveness of alternative treatments, and the morbidity of surgical resection. In general, the indications for any major surgical procedure include the potential for cure, prolongation of survival and palliation of symptoms. For metastatic tumors to the liver in selected cases the cure rate may be over 50% for colorectal cancer, 1 but will be exceedingly rare for other histologies such as gastric cases, and melanoma and sarcoma. Small metastases to the liver generally do not cause symptoms (except for hormone secreting neuroendocrine tumors) and, therefore, palliation of symptoms is not a common indication for management of these lesions. Does resection of a small solitary hepatic metastasis prolong survival in cases where the patient is likely to develop widespread metastases in the future Is there any harm in allowing a tumor to go untreated for a period of time, knowing that with close followup the resection option may still be possible in the future Do metastases metastasize such that a delay in management may obviate the curative option Unfortunately, all of these difficult issues are only addressed by sparse data in the literature. The risk and extent of the surgical procedure plays a significant role in the decision making for management of small hepatic metastases. It is more reasonable to excise an enlarged subcutaneous lymph node for metastatic cancer than it is to perform a hepatic lobectomy when the chance of benefit is low in both cases. As other less invasive ablative options become routine therapy, it may be reasonable to consider these options in cases where surgical resection is unreasonable. These alternative options include percutaneous approaches at ablation such as radiofrequency ablation and percutaneous alcohol injection. If the risks, discomfort, and hospital stay are truly minimal, then it becomes reasonable to consider local treatment of these lesions, even with a small chance of overall benefit to the patient. This chapter will provide an overview of the data on survival benefit after resection of hepatic metastases and the techniques of surgical management. A brief discussion of minimally invasive and percutaneous procedures for management of small solitary hepatic metastases will follow. In addition, a discussion of the role for adjuvant therapy Small solitary hepatic metastases: when and how Survival results for hepatic metastasectomy While the purpose of this chapter is not to provide an in-depth review of the results of hepatic metastasectomy, a general sense of expected cure rate and prolongation of survival after hepatic metastasectomy for various histologies is required in order to make an informed decision regarding resection of small hepatic metastases. Colorectal metastases Colorectal cancer, compared to other histologies, is more likely to present as disease isolated to the liver. After resection of solitary metastases from colorectal cancer, 5-year survival ranges from 30% to 47%. The size of the lesion is expected to affect prognosis and, therefore, the actual results for small solitary hepatic metastases may be even better than the numbers reported in Table 6. Liver resection for hepatic colorectal metastases is, therefore, safe and effective, and may be curative. Surgical management of hepatobiliary and pancreatic disorders 128 Neuroendocrine metastases For cancers of other than colorectal origin, patients with hepatic metastases from neuroendocrine tumors have been thought to be the most likely to benefit from surgical resection. Certainly, if the tumor were symptomatic for either hormonal or physical reasons, resection should be considered even though cure is unlikely. Because of the indolent nature of these tumors, durable palliation can be achieved with cytoreduction. Five-year survival rates for untreated hepatic metastases from neuroendocrine tumors have ranged from 13 to 54%. We and others 16 have adopted a very aggressive approach even for asymptomatic tumors based only on retrospective data. Certainly for small hepatic metastases, aggressive surgical resection is indicated, while it is acknowledged that definitive proof of its benefit may never be achieved. Non-colorectal, non-neuroendocrine metastases For histologies other than colorectal or neuroendocrine cancer, the utility of hepatic metastasectomy is not as obvious. For these tumors the liver is rarely the sole site of disease; liver metastases are rarely the ultimate cause of death, nor does it contribute significantly to symptoms prior to death. Nevertheless, selected cases of disease isolated to the liver after a long disease-free interval raise the possibility of a single site of metastatic disease that could be cured with surgical therapy. Breast cancer Many reviews have been published on hepatic metastasectomy for breast cancer. Due to the high incidence of breast cancer and the frequency of liver metastases for this histology, the first site of metastases is frequently observed to be hepatic. In highly selected patients, favorable results of section of such liver metastases have been reported. The survival rates reported are actuarial survival rates and the actual cure rate is much lower. At most, hepatic metastasectomy for breast cancer should be Small solitary hepatic metastases: when and how It may delay the development of symptoms and prolong survival, but it has very little chance of curing the disease. Sarcoma Similarly, hepatic resection for sarcoma metastases may be associated with long-term survival in highly selected patients, but it is unlikely to result in cure. In a series of 14 hepatic resections for metastatic sarcoma, recurrence was found in all patients during follow-up, and 11 of 14 failed in the liver. Melanoma Metastatic cutaneous melanoma to the liver has been resected with long-term survival, Surgical management of hepatobiliary and pancreatic disorders 130 but these tumors also ultimately recur. Only in highly selected cases is it appropriate to consider resection of cutaneous melanoma. Ocular melanoma preferentially metastasizes to the liver and the majority of patients die of liver failure as a direct result of tumor progression. Anecdotal reports exist of long-term survival after metastasectomy for ocular melanoma, 23 although these tumors are also almost always multifocal and resection of what appears to be a solitary metastasis is most often associated with liver recurrence. These hepatic metastases may show up many years after the treatment of the primary tumor. A long disease-free interval reflects a slow tumor doubling time, and suggests resection may achieve durable palliation. Usually in this disease, however, the appearance of a solitary liver metastasis is merely a precursor of the later appearance of multiple metastases. Other gastrointestinal cancers In general, hepatic metastasectomy for gastrointestinal primaries other than colorectal is not associated with prolonged survival. For tumors such as esophageal, gastric, small bowel, and pancreatic cancer the pattern of spread includes regional lymph nodes, the peritoneal cavity, and lung metastases in addition to liver metastases. It is unlikely that these patients will die of liver failure as a result of progression of hepatic metastases, but instead, suffer other gastrointestinal sequelae from extrahepatic tumor progression. A major operative procedure can be of significant detriment to these patients with aggressive cancers where survival is expected to be of the order of weeks to months. Nevertheless, even for these tumors selected cases exist where one might consider resection, and the literature contains anecdotal reports of long-term survivors after liver resection. For small solitary hepatic metastases, where many months of growth would still not preclude resection, the question is whether a waiting period would allow for further spread of the tumor from the metastatic deposit itself. If metastatic tumors were unable to Small solitary hepatic metastases: when and how If, however, metastases are able to spread during that waiting period, then the chance of potential cure may be adversely affected by the delay in definitive treatment. Unfortunately, it is clear that metastatic tumors do have the potential to metastasize themselves, and this must be considered when recommending observation alone. Experimental evidence suggests that cells from spontaneous metastases are more likely to metastasize than cells populating the parent neoplasm. Therefore, excision of liver tumors before they spread to regional lymph nodes would be advantageous. A recent paper examined the incidence of satellite micrometastasis in colorectal liver metastases by careful histologic examination of resection specimens and found that 56% of specimens had micrometastases as far as 3. As discussed previously, the presence of satellitosis is an important independent poor prognostic factor. It may be that a delay in resection allows for the development of satellitosis, which negatively impacts on prognosis. On the other hand, the presence of satellitosis may be an indicator of biologic aggressiveness which portends a poor prognosis regardless of when the tumor is resected. Patient selection Colorectal metastases In order to decide when surgical resection is reasonable for small solitary hepatic metastases, it is important to review prognostic factors which are independent of size and number that may influence the decision regarding management of these tumors. Many studies have examined data on prognostic factors for outcome after hepatic resection for colorectal metastases. The time to development of liver tumor after resection of the primary, pathologic margin, stage of the primary tumor, tumor number, carcinoembryonic antigen levels, satellitosis, extrahepatic disease, and positive surgical margin have all been shown to predict survival after hepatic resection for colorectal metastases independent of size. Even the presence of perihepatic lymph nodes portends a poor prognosis and generally is felt to be a contraindication to resection.
New York State Medicaid does not intend to pay more than the acquisition cost of the drug dosage medications post mi buy diltiazem 60 mg low price, as established by invoice symptoms of flu generic 180mg diltiazem amex, to the practitioner medicine encyclopedia order diltiazem 180mg overnight delivery. Regardless of whether an invoice must be submitted to Medicaid for payment medicine 0552 discount 60mg diltiazem with visa, the practitioner is expected to limit his or her Medicaid claim amount to the actual invoice cost of the drug dosage administered medications of the same type are known as buy generic diltiazem online. The patient must be 21 years of age or older at the time to consent to sterilization treatment 2nd degree burn 180 mg diltiazem. In cases of premature delivery and emergency abdominal surgery, consent must have been given at least 72 hours prior to sterilization. To indicate a bilateral surgical procedure was done add modifier -50 to the procedure number. One claim Version 2019 Page 5 of 257 Physician Procedure Codes, Section 5 Surgery line is to be billed representing the bilateral procedure. Reimbursement will not exceed 125% of the maximum State Medical Fee Schedule amount. Note: Unless otherwise designated, this modifier may only be appended to procedures/services listed in the 69999 code series. Such circumstances may be identified by each participating physician with the addition of the modifier -66 to the basic procedure number used for reporting services. When this subsequent procedure is related to the first, and requires the use of the operating room, it may be reported by adding the modifier -78 to the related procedure. This circumstance may be Version 2019 Page 6 of 257 Physician Procedure Codes, Section 5 Surgery reported by adding the modifier -79. The obtaining of tissue for pathology during the course of these procedures is a routine component of such procedures. This obtaining of tissue is not considered a separate biopsy procedure and is not separately reported. The use of a biopsy procedure code (eg, 11102, 11103, 11104, 11105, 11106, 11107) indicates that the procedure to obtain tissue soley for diagnostic histopathologic examination was performed independently, or was unrelated or distinct from other procedure/service provided at that time. Biopsies performed on different lesions or different sites on the same date of service may be reported separately, as they are not considered components of other procedures. Excision is defined as full thickness (through the dermis) removal of a lesion, including margins, and includes simple (non-layered) closure when performed. The excised diameter is the same whether the surgical defect is repaired in a linear fashion, or reconstructed (eg, with a skin graft). The closure of defects created by incision, excision, or trauma may require intermediate or complex closure. Excision is defined as full-thickness (through the dermis) removal of a lesion including margins, and includes simple (non-layered) closure when performed. Code selection is determined by measuring the greatest clinical diameter of the apparent lesion plus that margin required for complete excision (lesion diameter plus the most narrow margins required equals the excised diameter). When frozen section pathology shows the margins of excision were not adequate, an additional excision may be necessary for complete tumor removal. Use only one code to report the additional excision and re-excision(s) based on the final widest excised diameter required for complete tumor removal at the same operative session. To report a re-excision procedure performed to widen margins at a subsequent operative session, see codes 11600-11646, as appropriate. Wound closure utilizing adhesive strips as the sole repair material should be coded using the appropriate E/M code. This includes local anesthesia and chemical or electrocauterization of wounds not closed. Single layer closure of heavily contaminated wounds that have required extensive cleaning or removal of particulate matter also constitutes intermediate repair. Necessary preparation includes creation of a defect for repairs (eg, excision of a scar requiring a complex repair) or the debridement of complicated lacerations or avulsions. Complex repair does not include excision of benign (11400-11446) or malignant (11600-11646) lesions. Instructions for listing services at time of wound repair: Version 2019 Page 14 of 257 Physician Procedure Codes, Section 5 Surgery 1. The repaired wound(s) should be measured and recorded in centimeters, whether curved, angular or stellate. When multiple wounds are repaired, add together the lengths of those in the same classification (see above) and from all anatomic sites that are grouped together into the same code descriptor. For example, add together the lengths of intermediate repairs to the trunk and extremities. Do not add lengths of repairs from different groupings of anatomic sites (eg, face and extremities). Also, do not add together lengths of different classifications (eg, intermediate and complex repairs). Decontamination and/or debridement: Debridement is considered a separate procedure only when gross contamination requires prolonged cleansing, when appreciable amounts of devitalized or contaminated tissue are removed, or when debridement is carried out separately without immediate primary closure. Involvement of nerves, blood vessels and tendons: Report under appropriate system (Nervous, Cardiovascular, Musculoskeletal) for repair of these structures. Simple ligation of vessels in an open wound is considered as part of any wound closure. Simple exploration of nerves, blood vessels or tendons exposed in an open wound is also considered part of the essential treatment of the wound and is not a separate procedure unless appreciable dissection is required. If the wound requires enlargement, extension of dissection (to determine penetration), debridement, removal of foreign body(s), ligation or coagulation of minor subcutaneous and/or muscular blood vessel(s), of the subcutaneous tissue, muscle, fascia, and/or muscle, not requiring thoracotomy or laparotomy, use codes 20100-20103, as appropriate. When applied in repairing lacerations, the procedures listed must be developed by the surgeon to accomplish the repair. They do not apply when direct closure or rearrangement of traumatic wounds incidentally result in these configurations. Skin graft necessary to close secondary defect is considered an additional procedure. The primary defect resulting from the excision and the secondary defect resulting from flap design to perform the reconstruction are measured together to determine the code. When a primary procedure such as orbitectomy, radical mastectomy or deep tumor removal requires skin graft for definitive closure, see appropriate anatomical subsection for primary procedure and this section for skin graft or skin substitute. Repair of donor site requiring skin graft or local flaps is to be added as an additional procedure. Codes 15002 and 15005 describe burn and wound preparation or incisional or excisional release of scar contracture resulting in an open wound requiring a skin graft. Version 2019 Page 17 of 257 Physician Procedure Codes, Section 5 Surgery these codes are not intended to be reported for simple graft application alone or application stabilized with dressings (eg, simple gauze wrap) without surgical fixation of the skin substitute/graft. When services are performed in the office, the supply of the skin substitute/graft should be reported separately. Regions listed refer to donor site when tube is formed for later transfer or when delay of flap is prior to transfer. Procedures 15570-15738 do not include extensive immobilization, (eg, large plaster casts and other immobilizing devices are considered additional separate procedures) Repair of donor site requiring skin graft or local flaps is considered an additional separate procedure. Codes 16020-16030 include the application of materials (eg, dressings) not described in 15100. Lesions include condylomata, papillomata, molluscum contagiosum, herpetic lesions, warts (ie, common, plantar, flat), milia, or other benign, pre-malignant (eg, actinic keratoses), or malignant lesions. It requires a single physician to act in two integrated but separate and distinct capacities: surgeon and pathologist. If either of these responsibilities is delegated to another physician who reports the services separately, these codes should not be reported. The Mohs surgeon removes the tumor tissue and maps and divides the tumor specimen into pieces, and each piece is embedded into an individual tissue block for histopathologic examination. Thus a tissue block in Mohs surgery is defined as an individual tissue piece embedded in a mounting medium for sectioning. Biopsy procedures may be percutaneous or open, and they involve the removal of differing amounts of tissue for diagnosis. The open excision of breast lesions (eg, lesions of the breast ducts, cysts, benign or malignant tumors), without specific attention to adequate surgical margins, with or without the preoperative placement of radiological markers, is reported using codes 19110-19126. Partial mastectomy procedures (eg, lumpectomy, tylectomy, quadrantectomy, or segmentectomy) describe open excisions of breast tissue with specific attention to adequate surgical margins. Partial mastectomy procedures are reported using codes 19301 or 19302 as appropriate. Documentation for partial mastectomy procedures includes attention to the removal of adequate surgical margins surrounding the breast mass or lesion. Version 2019 Page 26 of 257 Physician Procedure Codes, Section 5 Surgery Total mastectomy procedures include simple mastectomy, complete mastectomy, subcutaneous mastectomy, modified radical mastectomy, radical mastectomy, and more extended procedures (eg, Urban type operation). Excisions or resections of chest wall tumors including ribs, with or without reconstruction, with or without mediastinal lymphadenectomy, are reported using codes 19260, 19271, or 19272. Codes 19260-19272 are not restricted to breast tumors and are used to report resections of chest wall tumors originating from any chest wall component. The services listed below include the application and removal of the first cast or traction device only. Subsequent replacement of cast and/or traction device may require an additional listing. This terminology is used to describe procedures that treat fractures by three methods: 1) without manipulation; 2) with manipulation; or 3) with or without traction. In this procedure, the fracture fragments are not visualized, but fixation (eg, pins) is placed across the fracture site, usually under x-ray imaging. The type of fracture (eg, open, compound, closed) does not have any coding correlation with the type of treatment (eg, closed, open or percutaneous) provided. The codes for treatment of fractures and joint injuries (dislocations) are categorized by the type of manipulation (reduction) and stabilization (fixation or immobilization). These codes can apply to either open (compound) or closed fractures or joint injuries. Skeletal traction is the application of a force (distracting or traction force) to a limb segment through a wire, pin, screw or clamp that is attached (eg, penetrates) to bone. Skin traction is the application of a force (longitudinal) to a limb using felt or strapping applied directly to skin only. External fixation is the usage of skeletal pins plus an attaching mechanism/device used for temporary or definitive treatment of acute or chronic bony deformity. Codes for obtaining autogenous bone grafts, cartilage, tendon fascia lata grafts or other tissues, through separate incisions are to be used only when the graft is not already listed as part of the basic procedure. To report, list only the primary surgical procedure performed (eg, sequestrectomy, deep incision). These codes describe surgical exploration and enlargement of the wound, extension of dissection (to determine penetration), debridement, removal of foreign body(s), ligation or coagulation of minor subcutaneous and/or muscular blood vessel(s), of the subcutaneous tissue, muscle fascia, and/or muscle, not requiring thoracotomy or laparotomy. If a repair is done to major structure(s) or major blood vessel(s) requiring thoracotomy or laparotomy, then those specific code(s) would supersede the use of codes 20100 20103. To report Simple, Intermediate or Complex repair of wound(s) that do not require enlargement of the wound, extension of dissection, etc. Codes 21076-21089 should only be used when the physician actually designs and prepares the prosthesis (ie, not prepared by an outside laboratory). For bone grafts in other Musculoskeletal sections, see specific code(s) descriptor(s) and/or accompanying guidelines. Example: Posterior arthrodesis of L5-S1 for degenerative disc disease utilizing morselized autogenous iliac bone graft harvested through a separate fascial incision. To report instrumentation procedures performed with definitive vertebral procedure(s), see codes 2284022855,22859. Instrumentation procedure codes 22840-22848,22853,22854,22859 are reported in addition to the definitive procedure(s). Example: Posterior arthrodesis of L4-S1, utilizing morselized autogenous iliac bone graft harvested through separate fascial incision, and pedicle screw fixation. Vertebral procedures are sometimes followed by arthrodesis and in addition may include bone grafts and instrumentation. When arthrodesis is performed addition to another procedure, the arthrodesis should be reported in addition to the original procedure. Examples are after osteotomy, fracture care, vertebral corpectomy and laminectomy. Since bone grafts and instrumentation are never performed without arthrodesis, they are reported as add-on codes. Example: Treatment of a burst fracture of L2 by corpectomy followed by arthrodesis of Ll-L3, utilizing anterior instrumentation Ll-L3 and structural allograft. A vertebral interspace is the non-bony compartment between two adjacent vertebral bodies, which contains the intervertebral disc, and includes the nucleus pulposus, annulus fibrosus, and two cartilagenous endplates.
Also medications beginning with z cheap 60 mg diltiazem with visa, crying will increase the amount of air in the There is a television showing short cartoons (Fig medications 25 mg 50 mg 180 mg diltiazem for sale. Other types of distracting to be fasting for an examination of the upper abdomen treatment diabetic neuropathy buy diltiazem 180 mg line, the items can be oered symptoms 7 days after conception discount diltiazem 60mg line. At the Royal Belfast Hospital for Sick session should be planned for as early as possible in the mornChildren symptoms acid reflux buy 180 mg diltiazem free shipping, a collage has been made with medical supplies ing medications kidney disease buy 180mg diltiazem free shipping. It is also worth having a quiet corner for very ill or injured children and bedridden patients who are not interested in this kind of distraction. Having a baby changing area in the changing room will allow parents to dress and undress their infant, thus improving the patient flow (Fig. The room should be large enough to accommodate a child along with the parents, siblings, and strollers, and there Fig. Paterson, should be enough room to exchange the couch for an inpatient Royal Belfast Hospital for Sick Children, Belfast, Northern Ireland. The room temperature should be warm enough for partially undressed patients; an infrared lamp can add extra warmth for newborns, who lose heat easily when undressed. Adolescents should be given the choice of having their any previous examinations, and the clinical information delivered parents present during the scan or not. It is also important in this short introducIt is important for the radiologist to build a good rapport with tion to take a short history and ask questions about what is worthe child and parents before starting the examination. If all peorying the child and/or the parents and what has been previously ple involved feel at ease, the chances of a successful diagnostic discussed with the referring physician. Use this It is usually the technician or radiology assistant who will time also to tell them that you will need to concentrate during invite the patient and parents into the room. This person will the examination but that you will inform them of the results introduce himself or herself and once again explain the procewhen the scan is finished, if they wish. When hearing the results and some explanation from you, whereas you walk into the scanning room and introduce yourself propothers may want to wait for the appointment with the referring erly to both the child and the parents, make sure the child is physician if there are no urgent matters to be dealt with. Be honest about what will sary to undress the child completely; pulling up tops and looshappen; an ultrasound scan is a painless test unless the region ening trousers or skirts is usually sucient. An adjustable position in height will allow children to climb on the couch or bed by themselves, which will give them a feeling of being in control (Fig. A large couch allows flexibility in positioning, and mothers can lie down next to their infants to breast-feed them and com1. A parent can lie on the couch Sedation is almost never needed for ultrasonography, although together with the child or sit next to you with the child on his if the child is young and too restless for the examination of a or her lap (Fig. It also helps the child from getting For abdominal examinations, an empty stomach is necessary bored lying on his or her back for more than 10 minutes. Babies can become very restless when hungry, good to have an arsenal of distracting toys at hand for the younmaking this examination dicult. Some children will feel more secure be present; make sure you have someone (a radiology assistant and in control if they can hold the transducer together with the or play therapist) to help you hold and entertain the child while doctor (Fig. Older children can be distracted 5 Examining the Child and Creating a Child-Friendly Environment Fig. However, distraction should not be forced upon a to make sure there is no delay in action (surgery, more tests, or child who is very upset or in pain. If there is enough space in your department, you may want to Adolescents may not ask questions for fear of appearing have a private room as an extension to the ultrasound scanning stupid. It can be used to discuss more complex or serious results in private when this discussion cannot wait, and a Tips from the Pro pediatric specialist can be called in to see the patient there Schedule ultrasound examinations for children wisely. Parents might prefer to hear the results from you Enter the examination room well informed and prepared. When the results of the test are normal, it will be easy to Have distraction tools at hand and/or have someone to reassure the parents and prevent days of worrying before the help you. Decreasing Recommended Readings pediatric patient anxiety about radiology imaging tests: prospective evaluation of an educational intervention. The wavelength , however, is related to sound is relatively inexpensive, noninvasive, and portable; it the medium by the following equation: has good spatial and temporal resolution; and it is safe. Ultrac sound imaging is based on the use of the echo of a sound wave m 2:2 f to produce an image of the insonated area. They used a transmission technique, similar to the technique used in X-ray imaging. In Just like visual light, sound breaks and reflects on discontinu1949, the first pulse echo was described. In pressure that is reflected on an interface and is given by the 1979, Professor Bom in conjunction with Professor Wladimiro, following equation: an obstetrician, introduced the Minivisor, the first portable ultrasound imager. The techniques evolved into applicawith Pi and Pr representing the incident pressure amplitude tions like life 3D and elastography, and the developments are (height) and the reflected pressure amplitude, respectively. It is proportional to the square of the pressure Ultrasound is defined as sound having a frequency higher than amplitude: 20kHz. In case of a perpendicular incidence, the intensity reflection Ultrasonic waves are longitudinal compression waves. Longicoecient thus becomes: tudinal means that the movement of the particles of the 2 medium is parallel to the direction of the wave movement. Here, the Ir Z2 Z1 movement of the particles is perpendicular to the direction of the wave. In longitudinal pressure waves, the movement of the particles leads to regions of compression and expansion correTable 2. No energy is transmitted small objects in a tissue, about the size of the wavelength or through the boundary. Nonspecular reflection is also called diuse reflection ence between Z1 and Z2 (Z1<<Z2 or Z1>>Z2). This means that the intensity of backscatleads to reflection coecients in the order of 0. This means ter, the part of the scattered signal that can be detected by the that 2% of the intensity of an incidence wave reflects on the ultrasound system, is quite small. Note that without these small dierences in the acoustic impedance of biomaterials, ultrasound imaging Attenuation would not be possible. Scattering and energy absorption in the tissue cause an attenuation of the ultrasound beam. This attenuation occurs exponenRefraction tially with the distance that the ultrasound wave travels As seen in Fig. The relative intensity in decibels is defined C2 as follows: At an interface from fat to muscle, we get sin i =1,450/1,600. The logarithmic relation A smooth boundary between two media, with the dimensions compresses the values of the intensity ratio into a more manof the boundary much larger than the wavelength of the ageable number range. The change in frequency due to the Doppler eect, also called the Doppler shift, is given by the following equation: 2 A fsend A v Fig. In daily practice, the Doppler shift and thus the velocity profile can be presented we hear the Doppler eect when the siren of an ambulance in a Doppler spectrogram (Fig. In ultrasound imaging, we encounter moving objects such as this lies in the audible range. The cells through a loudspeaker can be of help for the positioning of the thus become transmitters of sound (the echo). The wavelength on the left is blood flow in the umbilical arteries can be monitored by acoustic smaller than the wavelength on the right. Perpendicular to the direction of movement changes in Doppler shift patterns, and these can easily be (up and down), no change in wavelength occurs. This simple but very eective ultrasonic device there is no change in frequency in these directions. The longer it takes for an echo to arrive, the farther away the boundary that caused this echo. With knowledge of the direction of the incident pulse, information about the spatial position of the boundary is obtained. The time between repetitive pulses determines the maximal distance from which echoes can be processed. The intensity of the echo tells something about the change For a typical ultrasound Doppler measurement, fsend is known in acoustic impedance at the boundary. The angle of insonation is set on the console information about the anatomical structures that form the of the ultrasound machine. This leads to a wide dynamic range of intensities measurements, the angle of insonation should be kept as small of these echoes. The logarithmic relation compresses the values of the Continuous Wave Doppler intensity ratio into a more manageable number range. In image Continuous wave Doppler transmits and receives ultrasound construction, this means that a huge range of echo intensities continuously. The velocity can easily be determined by extraccan be represented within the limited amount of gray notes at tion of the Doppler shift through demodulation of the ultraour disposal. The amplitudes of these echoes are plotted Pulsed Wave Doppler against the distance from the probe. The intensity of the echo is represented is related to the pulse repetition frequency according to the in gray levels. In cardiology, it is used in the evaluation of heart valves and other heart anatomy. After a certain time, the pulse repetition time, when no echoes are expected to be received anymore, the next pulse is generated, and so on. The colors overlying the B-mode image represent velocity Linear Array values at that particular spot. The underlying calculations are the linear array transducer consists of an array of crystals. In power Doppler, just the total strength of the Sequentially, a group of adjacent crystals are fired, resulting in Doppler signal (power) is used for color representation. This dramatically improves sensiThen, the group of crystals are shifted one or more elements tivity. The shorter computing time can be translated into a higher and another scan is performed, generating the next line of echo temporal resolution and/or a higher spatial resolution. Thus, the ultrasound beam sequentially sweeps Power Doppler procedures are little aected by the angle of across the region of interest. It is superior in its visualization of approximately equal to the number of crystals (Fig. Mounting the array of crystals on a flat transducer surface produces a rectangular image. The width of the image and number of scan lines are the same at all tissue levels. The density of the scan lines 15 Physics and Artifacts Phased array transducers are used in cases with a small entrance window, such as in neonatal brain imaging, in which the width of the neonatal fontanel can be a limiting factor. Axial resolution depends on the wavelength of the ultradecreases with increasing distance from the transducer. In a phased array transducer, unlike in a linear array transducer, all Lateral resolution is the minimum distance that can be discrystals are simultaneously used to generate an ultrasound beam. Lateral resolution is related to the width of the the delay in firing of individual crystals. Some important assumptions are the following: the width of the sound bundle is infinite. Failure to comply with these assumptions leads to artifacts such as those discussed in the next sections. Because of the Elevational resolution or slice thickness is the thickness of the low attenuation, the echoes of distal structures have a relatively ultrasound beam. Enhancement occurs distal to fluid-filled cavities thickness is related to the height of the crystals, in much the such as the gallbladder or cysts. It can also be seen deep to very same way as lateral resolution is related to the width of the homogeneous tissue. It arises when an ultrasound pulse is trapped An artifact is defined as an incorrect display of anatomy. Part are many distinguishable types of artifacts in ultrasound imagof the pulse is reflected between the boundaries, thus causing it ing. The delay of these echoes is related to the number of times that the Aliasing pulse was reflected in its trap. It takes these echoes longer to Aliasing is a common artifact in pulsed wave Doppler. In the When a highly reflective surface is distal to an object, ghosts of Doppler spectrogram, aliasing appears as in Fig. In the ghost is generated by multiple reflections caused by the color Doppler imaging, aliasing and turbulence look quite simisame phenomenon as described with the reverberation artifact.
The urgency of treatment and the nature of resuscitation depend on the amount of blood loss treatment of lyme disease purchase diltiazem 180mg on line, the likely cause of the bleeding medications safe in pregnancy order diltiazem with visa, and the underlying health of the patient medications resembling percocet 512 60 mg diltiazem with mastercard. Early identification of colorectal cancer is important in preventing cancer-related morbidity and mortality (colorectal cancer is second only to lung cancer as a cause of cancer-related death) medications breastfeeding purchase diltiazem 180mg mastercard. Rectal injuries and sexual abuse Key Objectives 2 List the key steps in the management of lower gastrointestinal bleeding in high-risk patients as resuscitation and assessment treatment yeast diaper rash generic 60mg diltiazem with mastercard, localization medications you cant take with grapefruit best purchase diltiazem, and diagnosis and treatment (early involvement of a gastroenterologist and surgeon is essential). Bleeding usually starts and stops unpredictably, but under certain circumstances may require immediate establishment of an airway and control of the bleeding. With massive hemoptysis/respiratory difficulty, once the patient is stabilized, refer promptly for bronchoscopy. Contrast the disproportionate amount of blood flow in the pulmonary arteries, almost the entire cardiac output but at low pressure, to the much smaller blood flow at high pressure through the bronchial arteries, usually one or two branches off the aorta for each lung. Despite this disproportion,>90% of the time, hemoptysis originates from the bronchial arteries. Identify the pulmonary arteries as supplying nutritive blood supply for the airways, hilar lymph nodes, visceral pleura, and some of the mediastinum. Persistent hematuria implies the presence of conditions ranging from benign to malignant. Anticoagulants (note that the incidence of hematuria in patients on anticoagulants is similar to that in patients not receiving anticoagulants) 2. Once the presence of hematuria has been established and urinary tract infection has been excluded, it is critical to the further investigation of the patient to determine whether the hematuria is glomerular in origin or extra-glomerular. An experienced physician examining the urine sediment best accomplishes this differentiation. This information should be discussed with the patient before recommending more invasive and/or expensive investigations. Because persistent hematuria implies the presence of conditions ranging from benign to malignant, it cannot be ignored or assumed to be benign. List and explain various clinical findings that predispose to nephrolithiasis such as hypercalciuria, hyperuricosuria, hyperoxaluria, hypocitraturia, dehydration, and pH changes. Outline the role of humoral immunity and cellular immunity in glomerulonephritis and the target antigen predominantly localized in the glomerulus. Outline the structural and functional consequences of immune deposit formation in glomeruli. Explain the mechanisms of glomerular damage by immune events involving the complement system, polymorphonuclear cells, platelets, macrophages, oxidants and proteases. Describe the manner in which macromolecules are prevented from entering Bowman space and the permeability changes that make entry possible. Under such circumstances, the diagnosis of hypertension is made only after three separate properly measured blood pressures. Appropriate investigation and management of hypertension is expected to improve health outcomes. Outline the effect of cardiac output and systemic vascular resistance on blood pressure. Discuss autoregulation and the eventual consequence of this process on blood pressure and systemic vascular resistance when cardiac output is increased. Causal Conditions (same as hypertension in younger patients, but if age > 50 years, secondary hypertension becomes more likely) 1. Secondary hypertension Key Objectives 2 Define hypertension in the elderly in a manner similar to younger patients; define pseudo-hypertension and white coat hypertension. These include structural changes (orientation of the laminar unit within the wall, elastin fibre fracture, composition of wall with increased collagen content) along with arterial pulse change, and explain the systolic and pulse pressure elevation in the elderly (elastic properties or diminished compliance of the walls of arteries). List factors contributing to the increased prevalence of hypertension in the elderly. Explain hypertensive encephalopathy (refers to the occurrence of cerebral edema caused by hyperperfusion when a sudden, severe rise in blood pressure exceeds the capacity of the afferent arterioles to auto regulate). Outline the mechanism of vascular injury when pressure exceeds autoregulation and the increase in pressure is transmitted to arterioles and capillaries, including role of renin-angiotensin. Explain the potential ischemic consequences of an excessive hypotensive response to therapy when autoregulation capacity is exceeded at the lower pressure end of the auto regulatory curve. Chronic hypertension complicates<5%, preeclampsia occurs in slightly>6%, and gestational hypertension arises in 6% of pregnant women. Preeclampsia-eclampsia (new hypertension and proteinuria after 20 weeks gestation) a. Preeclampsia superimposed on chronic hypertension and proteinuria, both present before 20 weeks (severe exacerbation of blood pressure, systolic>180 mmHg, diastolic>110 mmHg, in last half of pregnancy) c. Masked chronic hypertension (persists beyond 12 weeks postpartum) Key Objectives 2 Describe normal changes in blood pressure during pregnancy and define hypertension in pregnancy with these changes in mind. Outline the changes in utero-placental circulation (impaired trophoblast invasion and placental ischemia) that occur in preeclampsia. Outline later changes resulting from placental ischemia such as altered capillary permeability, intravascular inflammatory response, abnormal prostaglandin metabolism, and activation of endothelial cells and the coagulation system. Regardless of underlying cause, certain general measures are usually indicated (investigations and therapeutic interventions) that can be life saving. Myxedema, Addison, liver failure Key Objectives 2 Elicit clinical and laboratory information necessary to diagnose the correct type of hypotension/shock. Outline the effect of cardiac output and systemic vascular resistance on blood pressure and tissue perfusion. Describe the effect of prolonged, severe hypotension on systemic tissue perfusion (results in decreased oxygen delivery, deprivation, and eventual cellular hypoxia). List some derangement of critical biochemical processes (cell membrane ion pump dysfunction, intracellular edema, leakage of intracellular contents, inadequate regulation of intracellular pH) that result from cellular hypoxia. Latex Key Objectives 2 Differentiate anaphylaxis from conditions which are similar such as shock from other causes, other flush syndromes, restaurant syndrome, increased endogenous histamine production, acute respiratory failure syndromes, or non-organic syndromes such as panic attacks or Munchausen syndrome. Invasive (invasive ductal/lobular carcinoma, tubular, medullary, papillary, mucinous) 2. An appropriate and prompt evaluation is important in order to relieve anxiety, even though breast cancer is not generally considered a medical emergency. It is the responsibility of the primary care physician to be an advocate for the patient throughout the entire process of evaluation of the breast lump. The physician should learn about the proficiency of local consultants in order to communicate these facts to the patient. The patient needs to be followed very carefully, maximizing exchange of ideas at every step of the process until suitable resolution is achieved. Abnormal breast discharge (usually Uni ductal, bloody or serosanguineous) breast neoplasm, benign or malignant Key Objectives 2 Differentiate between galactorrhea and breast discharge. Primary gonadal failure (Klinefelter, enzymatic defects in testosterone synthesis, testicular infections, trauma, malnutrition/starvation, renal failure) ii. Inhibitors of testosterone synthesis/action (aldactone, cimetidine, flutamide) iii. Idiopathic Key Objectives 2 Differentiate between gynecomastia and breast carcinoma. Contrast pathophysiological mechanisms for gynecomastia (absolute increase in free estrogens compared to decreased endogenous free androgens, versus relative increase in free estrogen/free androgen ratio, as opposed to androgen insensitivity). An understanding of the patho-physiology and treatment of burns and the metabolic and wound healing response will enable physicians to effectively assess and treat these injuries. Communicate with the burn patients or their legitimate delegates in order to obtain consent or refusal to investigate or treat. Explain the potential outcome of the burn and available options; determine whether the patient can provide the information back to you in a coherent manner. Consult hospital ethics committees about continuing care in patients with burns so extensive that mortality approaches 100%. In patients with severe burns, avoid marginally beneficial investigations or therapies. Describe the local (necrosis, inflammation) and systemic (fluids and electrolytes, hypermetabolism) manifestations of thermal injury. Discuss the unique features of electrical injury in relation to skeletal muscle injury and potential effect on cardiac and renal function. This differentiation by physicians is important for both diagnostic and management reasons. Miscellaneous Key Objectives 2 Although not common, hypercalcemia can cause severe anatomic injury to the kidneys, and if severe, patients may develop hypercalcemic crisis. Formulate a management plan for hypercalcemia consistent with its causal condition. Outline the metabolism of calcium including absorption, various forms of calcium in the blood, deposition, resorption and excretion. Hypomagnesemia Key Objectives 2 Calculate a corrected calcium concentration in the presence of hypoalbuminemia before initiating any other investigation (0. Include the various hormones (parathyroid, calcitonin), vitamin D and calcium receptors affecting these processes. Contrast the action of furosemide and thiazide diuretics on renal calcium handling. Serum phosphate concentration is primarily determined by the ability of the kidneys to excrete dietary phosphate. As a consequence, balance is maintained unless the load is acute and excessive (>130 mmol/day). In the community, cardiac arrest most commonly is caused by ventricular fibrillation. As a consequence, operational criteria for cardiac arrest do not rely on heart rhythm but focus on the presumed sudden pulse-less condition and the absence of evidence of a non-cardiac condition as the cause of the arrest. Acquired (associated with ischemic injury from coronary atherosclerosis, hypertension, diabetes mellitus) i. Chest wall trauma Key Objectives 2 this ultimate medical emergency requires immediate treatment. However, in other situations, most ethicists believe that autonomy takes precedence over beneficence. As a consequence, physicians generally request decisions about resuscitation from patients and their families. This does not mean that physicians should not provide patients and families with their expert opinion on the advisability of the procedure. This would be akin to abandoning responsibility to protect patients against inappropriate therapy in favor of complete autonomy. Rather than absolute autonomy, a more balanced approach of enhanced autonomy or fiduciary role is considered appropriate. Informed consent is a process that requires the involvement of both patient and physician. It is required that the physicians provide an opinion regarding what is considered the proper course of action. Informed consent requires explanations by physicians to patients and other decision-makers that facilitate reaching a decision. Consequently, it is important to determine whether the patient had expressed intention for such donation through advanced directives. This may lead to exclusion of patients who might benefit from evolving neurological therapies as well as lost opportunities for potential organ donation for those patients who may be neurologically dead but not yet diagnosed. The process of making such decisions should include a careful definition and full discussion with family about the goals of therapy.
Purchase diltiazem amex. కంచిలోని బంగారు వెండి బల్లి వెనుకున్న రహస్యం ఏంటి || Kanchi Bangaru Venddi Balli Rahasyam.