Luvox
Phuoc T. Tran, M.D., Ph.D.
- Professor of Radiation Oncology and Molecular Radiation Sciences

https://www.hopkinsmedicine.org/profiles/results/directory/profile/0024208/phuoc-tran
When the solitary metastases lies near an intersegmental plane anxiety 6 months after giving birth order line luvox, two segments can be removed anxiety symptoms stories depression men order 50 mg luvox fast delivery. The caudate lobe (segment I) can be resected as an isolated segmentectomy when the tumor is confined to this lobe anxiety symptoms head pressure buy luvox without prescription. The intersegmental planes were then marked by electrocautery and a formal segmentectomy was performed with negative margins anxiety symptoms brain fog purchase luvox 50 mg without prescription. While an aggressive resection was indicated and performed anxiety symptoms muscle twitches 50 mg luvox, the patient can still undergo a formal left or right hepatic lobectomy in the future if indicated anxiety disorder symptoms dsm 5 quality luvox 100 mg. In a recent report of 270 wedge or segmental resections, the operative mortality was 0. While mortality rates are low, the complication rate for major hepatic resection is still relatively high, ranging from 20% to 50%. Even though these complications do not translate into a high mortality rate, they may affect recovery time and quality of life. While this is not a significant issue for patients expected to Surgical management of hepatobiliary and pancreatic disorders 136 undergo a long-term disease-free interval or cure, it may be significant for patients whose survival is expected to be of the order of months. For those patients with aggressive tumors who are likely to fail outside the liver in the near future, less invasive techniques which are associated with a lower complication rate and quicker recovery time are more appealing. They provide ideal alternatives to laparotomy and major liver resection for the treatment of small solitary hepatic metastases, since the small tumor is the most likely to be completely treated by ablation techniques. Percutaneous approaches to tumor ablation are even more attractive than laparoscopic procedures. Local injection of toxic agents such as ethanol has been shown to be effective for hepatocellular cancers, however these agents have not been proven for other histologies and are known to be poorly effective for colorectal cancer. Because the patient will likely begin to fail in multiple sites in the near future with limited survival potential, a laparotomy and hepatic resection was not considered reasonable. She was treated with Surgical management of hepatobiliary and pancreatic disorders 138 percutaneous radiofrequency ablation, achieving a good zone of necrosis encompassing the mass, and she spent only one day in the hospital with very minimal discomfort. How such procedures, which have low morbidity and which maintain quality of life, will factor in the treatment of patients with small hepatic metastases must be addressed by studies with sufficient follow-up to define the local recurrence rate. Adjuvant chemotherapy the role for adjuvant systemic chemotherapy after the removal of small solitary hepatic metastases is not well defined. Even for hepatic colorectal metastases, which are commonly treated with surgery, data on adjuvant chemotherapy after liver resection is sparse. Two retrospective studies have suggested a benefit of adjuvant systemic chemotherapy after metastasectomy, but others have not supported this. There are currently no data to support the use of irinotecan and oxaliplatin in an adjuvant setting, although studies are in progress. For patients with hepatic colorectal metastases, the most common site of tumor recurrence after liver resection is the remnant liver. Regional chemotherapy to treat the liver site is therefore a theoretically attractive option for adjuvant care. Although no difference was found between the groups, technical factors compromised this study such that only 34 of the 114 patients randomized to chemotherapy completed the adjuvant treatments. For non-colorectal, non-neuroendocrine histologies metastatic to the liver the most Surgical management of hepatobiliary and pancreatic disorders 140 likely cause of death will be related to the disease outside the liver, regardless of how the liver is managed. For patients who are likely to develop systemic metastases in the near future it may be reasonable to offer chemotherapy prior to resection. If the tumor responds then a resection will be performed with confidence that other micrometastatic disease may be effectively treated with chemotherapy. If the tumor does not respond and the liver remains the only site of metastatic disease, resection is performed with increased confidence conferred by the longer period of observation. If the patient advances systemically during chemotherapy then it is very unlikely that a resection would have been of benefit and the patient will have avoided the potential morbidity, pain, discomfort and recovery time of an hepatic resection. That patient can go on to obtain second-line chemotherapy, investigational chemotherapy, or have no additional treatment. Conclusions Algorithms for the management of small solitary hepatic metastases are shown in Figure 6. Both patient and tumor characteristics must be considered in making management decisions. Immediate ablation or resection should be performed in the setting of a clinical trial, and most appropriately a trial examining adjuvant therapy. When the cancer is found in an asymptomatic patient, a period of observation is not unreasonable because of the often indolent nature of these tumors. At resection, the principle should be to leave as much normal liver behind in order to minimize the risk of liver failure and in order to allow for repeat anatomic liver resections in the future for recurrent disease. Enucleation with positive margins is acceptable for treatment of this histology because resection is almost never curative, and such cytoreduction can provide significant and durable palliation with minimum risk. For patients with small, solitary, non-colorectal non-neuroendocrine tumors the most significant factor in terms of prognosis seems to be the diseasefree interval (Fig. For patients with a long disease-free interval from primary resection a curative surgical resection is indicated as the most effective means of therapy. While it may be still unlikely that these patients can be cured, they must be given the benefit of the doubt and the most optimal procedure performed. Patients with a short disease-free interval from a tumor with a poor prognosis should undergo a trial of chemotherapy if there is a known effective agent. If no effective agent exists (as is the case for most solid malignancies), then these patients are ideal for an Small solitary hepatic metastases: when and how This provides an advantage to observation alone, given the low but definite risk of the metastases spreading during the observation period. It will be psychologically more comforting to the patient to know that the lesion has been ablated, and risk, pain and recovery duration are minimal. Observation alone is also quite reasonable, but it is often not accepted by patients. Patients who have concomitant illnesses which make them poor operative candidates may be better served with a minimally invasive or percutaneous technique, even in the case of potentially curable metastases from colorectal cancer. Because of improvements in diagnostic techniques and the routine use of serum tumor markers, the detection of small solitary hepatic metastases from various tumors will likely increase in the future. A uniform approach to these patients such as that which is outlined in the treatment algorithm should be considered. Regional treatment strategies for unresectable primary or metastatic cancer confined to the liver. A retrospective study of the natural history of patients with liver metastases from colorectal cancer. Perioperative blood transfusion and determinants of survival after liver resection for metastatic colorectal carcinoma. Isolated liver metastases from neuroendocrine tumors: does resection prolong survival Hepatic metastases from soft-tissue Small solitary hepatic metastases: when and how Treatment of liver metastases from uveal melanoma by combined surgerychemotherapy. Hepatic resection for metastatic tumours from gastric cancer: analysis of prognostic factors. Synchronous, metachronous and multiple hepatic resections of liver tumors originating from primary gastric tumors. Hepatic resection for noncolorectal, nonneuroendocrine metastases: a fifteen-year experience with ninety-six patients. Enhanced metastatic potential of tumor cells harvested from spontaneous metastases of heterogeneous murine tumors. Prospective study of microscopic lymph node involvement of the hepatic pedicle during curative hepatectomy for colorectal metastases. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of patterns of recurrence. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Segment-oriented hepatic resection in the management of malignant neoplasms of the liver. Anatomic segmental hepatic resection is superior to wedge resection as an oncologic operation for colorectal liver metastases. One hundred consecutive hepatic resections: blood loss, transfusion and operative technique. Ultrasound-guided laparoscopic cryoablation of hepatic tumors: preliminary report. Multivariate analysis of a personal series of 247 consecutive patients with liver metastases from colorectal cancer: I. Adjuvant hepatic intra-arterial chemotherapy after potentially curative hepatectomy for liver metastases from colorectal cancer: a pilot study. Adjuvant hepatic artery infusion chemotherapy after curative resection of colorectal liver metastases. Results of a prospective randomized trial of continuous regional chemotherapy and hepatic resection as treatment of hepatic metastases from colorectal primaries. Randomized trial of surgery versus surgery followed by adjuvant hepatic arterial infusion with 5-fluorouracil and folinic acid for liver metastases of colorectal cancer. Hepatic arterial infusion of chemotherapy after resection of hepatic metastases from colorectal cancer. Among these patients, those with bilobar metastatic disease represent the biggest challenge for the surgeon. In the multicentric retrospective study of the French Association of Surgery, 1 the largest series of liver resections for colorectal metastases to date, of the 1818 patients treated with a curative resection 20% of the cases were bilobar. We shall try to answer the following questions: (1) Is it therefore justifiable to resect bilobar colorectal liver metastases Surgical resection is currently accepted as a safe, and also the only potentially curative treatment available for patients with colorectal liver metastases, offering a chance of long-term survival with rates ranging from 25% to 50% at 5 years. They allow bilobar resections with very low mortality (around 1%) and low morbidity. Furthermore, there is still a lack of enthusiasm among many physicians regarding surgical resection of liver metastases when they are multiple; many of them are clearly reluctant in the case of bilobar disease. Nevertheless, most studies in the literature show clearly that there is no difference in 5year survival rate between patients with solitary or fewer than four metastases, whether the location is unilobar or bilobar. The data showed, on multivariate analysis, that the following factors were associated with a significantly better prognosis: presence of fewer than four metastases, diameter of less than 5 cm (Tables 7. In contrast, unilobar versus bilobar location had no influence on survival in this group (Figure 7. In contrast to some reports where bilobar liver involvement was found to be associated with lower Figure 7. Uninodular type (A) compared to multinodular metastasis with satellite nodules (B). Moreover, the postoperative complication rate is similar in subjects with unilobar or bilobar involvement. This means that surgical excision of two or three metastases, for example, should be undertaken if technically feasible, whether they are located on one half of the liver and require a lobectomy or in both lobes and demand two separate resections. It also means that if complete resection of the secondary tumors can be achieved with a wedge resection there is no need to perform a larger hepatectomy, provided a 1 cm clearance of normal parenchyma is resected with the tumor. It was concluded that if complete resection of the tumor is mandatory, a margin less than 1 cm should not be considered as an absolute contraindication to surgery. In these situations, cryotherapy has been recommended to improve the proportion of negative resection margins; 18 however, the proximity of a metastasis to a large blood vessel compromises an adequate freezing margin. Finally, there is a strong argument in favor of segmentectomies or minor resections rather than extended resections if they can be undertaken safely. Indeed, recurrences will unfortunately occur in the majority of patients after the first liver resection. A clinical score predicting recurrences after hepatic resection for metastatic colorectal cancer has been established by Fong et al. Other studies tried to identify parameters that could help to select subpopulations of patients with recurrent liver metastases who have a better prognosis after repeat resections. Bozzetti 26 showed that patients with a disease-free interval greater than 1 year between the first and second liver resections had a greater disease-free survival after the second resection. However, in the largest series no parameter significantly related to outcome could be identified, 27 even for bilobar liver involvement. Several authors recommended an aggressive approach for patients with recurrent or multiple bilobar liver metastases from colorectal primaries. Surgical Management of hepatobiliary and pancreatic disorders 150 Pathophysiology of bilobar distribution Many studies have attempted to explain (1) the ability of some primary tumors to develop metastases, 32 and (2) the lobar distribution of these metastases in the liver. It has been suggested that right-sided colon cancers involve the right hepatic lobe more selectively while left-sided tumors involve the entire liver, according to streaming of flow in the portal vein.
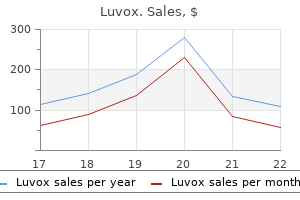
Those subjects who showed improved compliance and also had baseline higher bone lead content produced an overall reduction of 16 relieve anxiety symptoms quickly order luvox us. Similar positive findings came from a study in Mexico of 367 lactating women; however anxiety back pain purchase luvox 100mg free shipping, the maximal reduction in lead concentrations reached only 10% (Ettinger et al 2006) anxiety symptoms 24 7 purchase luvox overnight delivery. Nevertheless anxiety symptoms of menopause generic luvox 100mg amex, when considered together these results suggest that calcium supplementation may represent an important interventional strategy anxiety quotes best luvox 100 mg, albeit with a modest effect anxiety panic attacks buy 100 mg luvox with amex, for reducing infant lead exposure. Calcium in combination with the other ingredients reduces stomach acid and increases the rate of gastric emptying (Vatier et al 1996). In trials comparing H2 blockers with calcium carbonate tablets, calcium was found to be equipotent, yet delivered a more rapid response and shorter duration of action (Feldman 1996). A 2005 Cochrane review examining the effect of supplementary calcium on the incidence of colorectal cancer and the incidence or recurrence of adenomatous polyps included two double-blind, placebo-controlled trials with a pooled population of 1346 subjects. The reviewers concluded that while the evidence to date appears promising and suggests a moderate degree of prevention against colorectal adenomatous polyps, more research with similar findings is required before this can be translated into any preventative protocol (Weingarten et al 2005). Not included in the Cochrane review was a multicentre, placebo-controlled randomised study assessing the independent and joint effects of calcium supplementation and vitamin D status on adenoma recurrence in 803 subjects. Interestingly only those subjects with baseline vitamin D levels above the median (29. Similarly, high vitamin D status was not independently associated with risk reduction, but was protective in combination with calcium supplementation (Grau et al 2003). This notion is further supported by a number of studies demonstrating enhanced chemoprotection when high doses of calcium have been combined with dietary factors such as reduced fat and increased carbohydrate, fibre and fluid intakes (Hyman et al 1998, Rozen et al 2001, Schatzkin & Peters 2004). One significant development in our understanding has been the discovery of human parathyroid calcium-sensing receptors in the human colon epithelium, which function to regulate epithelial proliferation and differentiation. New in vitro studies suggest that expression of these receptors may be induced by the presence of extracelullar calcium and vitamin D, therefore promoting greater differentiation of the epithelial cells (Chakrabarty et al 2005) and inducing apoptosis (Miller et al 2005). The emerging evidence to date for a combined role of calcium, either dietary or supplemental, and vitamin D is strong and further elucidation of the independent and combined effects of these nutrients will assist in the development of preventative protocols. The authors temper their conclusion by stating that the quality of included trials was poor and the heterogeneity between trials means there is a tendency to overestimate the effects of treatment. Although dietary calcium appeared to have a larger effect than supplementation, the difference was not statistically significant. The clinical significance of these small effects has been questioned and the recommendation of calcium as a therapy for all types of hypertension appears premature (Kawano et al 1998). Some studies have proposed that it is only a particular subset of hypertension that demonstrates the greatest improvement with calcium. In recent years, ongoing international epidemiological data have continued to link low dietary calcium intake with a slightly increased risk of hypertension, such as the study by Geleijnse et al published in 2005. Additional findings that are attracting attention include epidemiologic links between markers of low calcium status or calcium metabolism abnormalities, hypertension and insulin resistance. In support of the possible link between these phenomena are the results of a Japanese study of 34 non-diabetic hypertensive and 34 non-diabetic normotensive women. Results showed that 73% of women reported improved symptoms while taking calcium supplementation whereas 15% preferred placebo. The premenstrual symptoms responding significantly to calcium supplementation were mood changes, water retention and premenstrual pain. In 1993, the American Journal of Obstetrics and Gynecology published a study that compared the effects of calcium (587 mg or 1336 mg) and manganese (1. Ten women with normal menstrual cycles were observed over four 39-day periods during the trial (Penland & Johnson 1993). The researchers found that increasing calcium intake reduced mood, concentration and behavioural symptoms generally and reduced water retention during the premenstrual phase. A more recent large, double-blind, placebo-controlled, randomised parallel-group study was conducted in the United States and supports the previous findings (ThysJacobs et al 1998). Symptoms were documented daily by the subjects based on 17 core symptoms and 4 symptom factors (negative affect, water retention, food cravings and pain). During the luteal phases of both the second and third treatment cycles, a significantly lower mean symptom score was observed in the calcium group. By the third treatment cycle, calcium treatment resulted in a 48% reduction in total symptom score compared with baseline, whereas placebo achieved a 30% reduction. The review brought together a broad range of trials dating back 10 years to the original findings demonstrated on hypertensive rats. Additional proposed actions include increased rates of faecal fat and energy excretion (14. Interestingly, these increased losses were not evident when high calcium and protein intake was combined (23%). One prolific researcher in this area is Zemel (2004, Zemel et al 2004, 2005a, b), who has published three small trials investigating the effects of dietary and supplemental calcium in patients for weight maintenance or weight loss. Australian researchers Bowen et al have also demonstrated similar results (2004). Zemel et al conclude that dietary calcium and, in particular, dairy based foods are the most effective form of calcium for weight loss and that results are significant within 12 weeks. In stark contrast to this, there have been a number of studies reporting negative results. A trial of isocaloric energy restricted diets in 54 overweight subjects with either low or high calcium intake from dairy products found that over 12 months there was no significant difference in weight loss between the two groups (HarveyBerino et al 2005). Finally caution is being encouraged by many authorities who are keen to remind researchers that epidemiological data have positively linked high dairy diets with a range of other conditions, most notably prostate cancer (Lanou 2005). A study comprised 120 men who experienced recurrent calcium oxalate stones as a sequel to idiopathic hypercalcuria and who were randomly assigned to either a low-calcium diet or low-animal-protein, low-salt normal-calcium diet and assessed for changes in frequency of stone formation. Results clearly showed reduced oxalate excretion in those on a normal calcium intake, as well as a greater decrease in calcium oxalate saturation (Borghi et al 2002). In another study of 14 healthy men, assessment of the influence of dietary calcium on the given amount of oxalate demonstrated that with the inclusion of additional calcium (1121 mg) urinary oxalate levels did not increase, while they did in the control group (Hess et al 1998). The view is that, rather than being a contributing factor for oxalate stones, dietary calcium, through its binding of oxalate in the gut, can minimise recurrence, and this is substantiated by other studies (Curhan et al 1997, Liebman & Chai 1997). No other effects on other blood lipids or blood pressure were observed (Bell et al 1992). Hypercalcaemia Increased serum calcium may be associated with anorexia, nausea and vomiting, constipation, hypotonia, depression and occasionally lethargy and coma. Prolonged hypercalcaemic states, especially if associated with normal or elevated serum phosphate, can precipitate ectopic calcification of blood vessels, connective tissues around joints, gastric mucosa, cornea and renal tissue (Wilson et al 1991). Only those interactions encountered with oral administration of calcium supplements will be included in this section. Monitor serum calcium and look for signs of hypercalcaemia, such as anorexia, polydipsia, polyuria, constipation and muscle hypertonia when using high-dose calcium supplements. Contributing risk factors are the presence of hyperparathyroidism or concurrent use of vitamin D. This will depend on the indication it is being used to treat; however, in most instances Calcium 164 long-term administration is required. In very high doses, calcium supplements can cause some side-effects, including constipation, but generally calcium is considered very safe and has a wide therapeutic range. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Long-term effect of calcium supplementation during pregnancy on the blood pressure of offspring: follow up of a randomised controlled trial. Cholesterol-lowering effects of calcium carbonate in patients with mild to moderate hypercholesterolemia. Milk, dairy fat, dietary calcium, and weight gain: a longitudinal study of adolescents. Comparison of two diets for the prevention of recurrent stones in idiopathic hypercalciuria. A high dairy protein, high-calcium diet minimizes bone turnover in overweight adults during weight loss. Effect of calcium supplementation on pregnancy-induced hypertension and preeclampsia. Five year study of etidronate and/or calcium as prevention and treatment for osteoporosis and fractures in patients with asthma receiving long term oral and/or inhaled glucocorticoids. Calcium sensing receptor in human colon carcinoma: interaction with Ca(2+) and 1,25-dihydroxyvitamin D(3). Effect of calcium and cholecalciferol treatment for 3 years on hip fractures in elderly women. Interaction between calcium intake and menarcheal age on bone mass gain: an eight-year follow-up study from prepuberty to postmenarche. Central hypervolemia does not invariably modulate calcium excretion in essential Calcium 165 hypertension. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Effect of supplementation of calcium and Vitamin D on bone mineral density and bone mineral content in periand post-menopause women A double-blind, randomized, controlled trial. Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. Influence of maternal bone lead burden and calcium intake on levels of lead in breast milk over the course of lactation. Biochemical effects of calcium supplementation in postmenopausal women: influence of dietary calcium intake. Comparison of the effects of over-the-counter famotidine and calcium carbonate antacid on postprandial gastric acid: A randomized controlled trial. Dietary fiber, potassium, magnesium and calcium in relation to the risk of preeclampsia. Impact of dietary and lifestyle factors on the prevalence of hypertension in Western populations. Vitamin D, calcium supplementation, and colorectal adenomas: results of a randomized trial. The influence of dietary and nondietary calcium supplementation on blood pressure: an updated metaanalysis of randomised controlled trials. Calcium and vitamin D status in the adolescent: key roles for bone, body weight, glucose tolerance, and estrogen biosynthesis. Dietary calcium supplements to lower blood lead levels in lactating women: a randomized placebo-controlled trial. Effect of antacids on mineral metabolism in persons with healthy kidneys: Doubleblind study using an antacid containing magnesium aluminum silicate hydrate. High-calcium intake abolishes hyperoxaluria and reduces urinary crystallization during a 20-fold normal oxalate load in humans. Effect of short-term high dietary calcium intake on 24-h energy expenditure, fat oxidation, and fecal fat excretion. Calcium supplementation in patients with essential hypertension assessment by office, home and ambulatory blood pressure. Double-blind, randomized trial of a synthetic triacylglycerol in formula-fed term infants: effects on stool biochemistry, stool characteristics, and bone mineralization. Data do not support recommending dairy products for weight loss [Letter to the Editor]. Vitamin D and calcium supplementation prevents osteoporotic fractures in elderly community dwelling residents: a pragmatic population-based 3-year intervention study. Calcium supplementation and bone mineral density in females from childhood to young adulthood: a randomized controlled trial. Calcium potentiates the effect of estrogen and calcitonin on bone mass: review and analysis. Lactation and bone development implications for the calcium requirements Calcium 167 of infants and lactating mothers. The pathogenesis of age-related osteoporotic fracture: effects of dietary calcium deprivation. Serum calcium and phosphorus associate with the occurrence and severity of angiographically documented coronary heart disease, possibly through correlation with atherogenic (apo)lipoproteins. The effect of sodium monofluorophosphate plus calcium on vertebral fracture rate in postmenopausal women with moderate osteoporosis: a randomized, controlled trial. Avoidance of vertebral fractures in men with idiopathic osteoporosis by a three year therapy with calcium and low-dose intermittent monofluorophosphate. Calcium supplements interact significantly with long-term diet while suppressing rectal epithelial proliferation of adenoma patients.
Order luvox 50mg visa. Can anxiety attacks happen to anyone and everyone?.

Young hypermetropes Hence anxiety explained order luvox in india, a point focus cannot be formed upon the are prone to develop latent convergent squint retina (Fig anxiety symptoms nausea order cheapest luvox and luvox. In general anxiety gif purchase luvox toronto, caused by abnormalities in the curvature of the presbyopia commences at an early age than usual cornea (curvature astigmatism) anxiety young children purchase 100 mg luvox amex. A hypermetropic eye is usually the curvature or centering of the lens can also smaller than the normal anxiety symptoms depersonalization cheap luvox 50 mg mastercard, particularly along the cause astigmatism anxiety symptoms confusion buy discount luvox 100mg. The diameter of the cornea is reduced matism occurs due to inequalities in the refractive and the anterior chamber is often more shallow index of different sectors of the lens (index than usual. Parallel rays are brought to a focus on the retina by an appropriate convex lens Fig. This is accepted as Theoretically, no eye is stigmatic as the vertical physiological and termed as astigmatism with-thecurvature of the cornea is greater than the rule. The most common cause of astigmatism often cause poor visual acuity but astigmatism against-the-rule is cataract surgery vision is not much impaired in mixed astigmatism from superior corneal, limbal or corneoscleral as the circle of least diffusion falls upon or near section in which the vertical meridian flattens due the retina. The patient sees distinct lines of the sionally, the axes are not at right angles but are fan in one direction (vertical or horizontal) and crossed obliquely; this condition is known as bithey appear tailed off or blurred in the other oblique astigmatism. Simple astigmatism, where one of the principal scar, penetrating injuries of the eye, keratoconus, meridians is emmetropic and the other is either lenticonus and immature cataract. The former is known with irregular astigmatism often suffers from as simple hypermetropic and the latter simple distorted vision and headache. Compound astigmatism, where both the princiTreatment pal meridians are either hypermetropic or A small degree of astigmatic error may not require myopic, the former is known as compound any optical correction. But in all such cases, if the hypermetropic and the latter compound myopic error causes asthenopic symptoms, a full optical astigmatism. All forms of regular astigmatism meridians is hypermetropic and the other can be corrected by cylindrical lenses or spheromyopic. In contrast, irregular astigmatism cannot be corrected by spectacle Clinical Features lenses due to irregularities in curvature of Generally, small astigmatic errors do not give any meridians. However, severe symptoms are the visual acuity does not improve in cases of found in cases of hypermetropic astigmatism irregular astigmatism with spectacle correction; wherein the accommodation is brought into play here toric contact lenses are of immense value. Errors of Refraction 33 Soft or rigid gas permeable toric lenses are size of the retinal images (aniseikonia) in the prescribed. The use of Large degrees of astigmatism following contact lens eliminates this defect. If the eye has cataract extraction and keratoplasty can be become amblyopic, the emmetropic eye is patched managed by laser in situ keratomileusis or and the patient is encouraged to use the ametropic conductive keratoplasty. Later, orthoptic relaxing incisions in the cornea, or limbal relaxing exercises should be given to develop binocularity. In all these Laser in situ keratomileusis has been tried with techniques the closer the incision to the center of satisfactory results in cases of anisometropia. It is significant when the difference Occasionally, the patient complains of throbbing between the refraction of the two eyes exceeds 2. A minor difference of refraction between the the main causes of asthenopia are: two eyes is not uncommon and it seldom gives 1. Binocular vision is usually mainmetropia and astigmatism tained if the difference between the two eyes does 2. In some cases, when one eye is optical center of a corrective lens emmetropic or moderately hypermetropic and the 3. It ultimately leads to amblyopia the causes of asthenopia must be identified and ex-anopsia (amblyopia due to disuse). The corrective of uniocular myopia, hypermetropia and unimeasures include correction of refractive error, ocular aphakia are important causes of anireplacement of inappropriate glasses, orthoptic sometropia. The Myopias: Basic Sciences and Clinical acceptable to the child due to difference in the Management. The objective determination of the refraction can be done either by objective optometry or retinoscopy and occasionally by keratometry. The optometers are automated computerized instruments which measure quickly the far point of the eye and give instantaneous printout of the refractive error of the subject screened in terms of sphere, cylinder, axis, interpupillary distance and other technical data. However, these readings cannot be blindly prescribed, as the subjective acceptance and tolerance significantly differ in practice owing to personal and instrumental errors. The the most commonly employed method for deterretinoscopy is a process by which the far point of mining the refraction objectively is retinoscopy or the eye is brought nearer to the eye, say at 1 meter, skiascopy. The basic principle of retinoscopy is that with the help of trial lenses placed in front of the when light is reflected from a mirror into an eye, eye under examination. Determination of the Refraction 35 It has already been explained that the emergent light rays are parallel in emmetropic, divergent in hypermetropic, and convergent in myopic eyes. We know that the far point of the myopic eye (1D) lies at 1 meter in front of the eye and the trial lenses can be employed to alter the vergence in front of the eye. His fundus is illuminated with the help of a mirror held by the examiner in his hand. The reflected light from the fundus is seen as a red reflex filling the pupillary area. If the mirror is tilted either upwards, downwards or to right or left, the reflex also appears to move. This illusionary movement of the reflex with the movement of the mirror depends upon the nature of the refractive status of the eye. If a plane mirror is used for retinoscopy at a working distance of 1 meter, the movement of reflex is in the same direction (with movement) to the movement of mirror in emmetropia, hypermetropia and myopia of less than 1 D, whereas the reflex moves in the opposite direction to the movement of the mirror in myopia of more than 1 D. If a concave mirror is used instead of a plane mirror and the other conditions remaining the same, the reflex moves in the opposite direction (against movement) to the movement of mirror in emmetropia, hypermetropia and myopia of less than 1 D but reflex moves in the same direction to Fig. This point is called neutral point or If an eye has a myopia of 1 D, the retinoscopic neutral reflex. An optometrist, while doing reflex at a distance of 1 meter with a plane mirror refraction, attempts to obtain this point by adding becomes neutral, i. Either the reflex appears bright difficult to obtain the neutral point, hence, a point or completely dark. This condition is created slight tilt of the mirror, disappears quickly and by adding a slightly higher power (+ 0. For bromide (2%), tropicamide (1%) or cyclopentolate example, in a hypermetropic individual if the (1%) to relax their accommodation during retinospoint of reversal is achieved with + 4 D sphere, copy. In such Retinoscopy is usually performed in a dark cases a correction must be made to compensate room. In high degree of the state of refraction of the eye when focused of ametropia, the reflex has a curved border, is for near vision is known as dynamic retinoscopy. But in low refractive error, Generally, near correction for a presbyope is the reflex is bright, with straight border and moves advised over a distant correction considering the rapidly. If the reflex moves with the mirror, progressively Keratometry is a technique which measures the stronger convex lenses are put in the trial frame curvature of the cornea with the help of an until a point of reversal is obtained. It is is equal in both the meridians, only spherical especially useful in the assessment of corneal correction is needed. Keratometry shadow becomes band-shaped, the edge of the is based on the fact that the front surface of the band being parallel to the axis of the neutralized cornea acts as a convex mirror and the size of the meridian. The mirror is then moved at right angles image of an object reflected by it varies inversely to the neutralized meridian and a point of reversal with its curvature. The instrument consists of two is obtained by adding the lenses in the trial frame. However, the mires are reflected on the cornea of the patient a cycloplegic is essential for the estimation of and one observes four images of the mires through refractive error in children as they have strong the telescope. A: Nonaligned mires, B: Aligned mires remain unchanged, there is no astigmatism. In the presence of astigmatism, the mires will overlap or separate, hence, readjustment is required. Generally, the mire is so constructed that each step corresponds to 1 D of astigmatism. The mires appear grossly distorted in irregular astigmatism and no useful reading can be obtained. The instrument discarded and the remaining two are adjusted in has 2 maneuverable prisms aligned vertically and such a way that they coincide with each other at horizontally. The radius of are 2 adjustable images, one above and one to the curvature and refractive power can be read from a left (Fig. The post-mydriatic test should be delayed for 2 weeks when atropine is used, for 48-72 hours if homatropine or cyclopentolate is applied and for a day following tropicamide-induced cycloplegia so that the physiological ciliary tone is restored. As a general rule, the weakest concave lens or the strongest convex lens (in myopia and hypermetropia, respectively) from the trial case (Fig. The same procedure is repeated for the occluded eye and finally the acceptance is verified binocularly. In this method, the patient is made myopic by 1 D by addition or subtraction from the retinoscopic findings. If the vision does not improve to 6/6, cylindrical lenses should be tried as per the retinoscopy. It is used for subjective refinement of determined by the use of either an astigmatic fan the axis and the power of the prescribed cylinder. If the patient formed on the retina, by increasing or decreasing is stigmatic, all the lines appear equally clear to the astigmatic ametropia. But if there is astigmatism, he sees some of To check the strength of the cylinder in the the lines more clearly than the others. In the presence of astigmatism, remains unchanged, the cylinder in the trial frame the patient will see some of the lines more sharply is correct. Concave cylinder is now added with its suitable alteration in the strength of the cylinder axis at right angles to the clearest line until all the is to be made. The green the correction of near vision should be preceded rays, having a short wavelength, are refracted by the distant correction and determination of more acutely and brought to a focus earlier than near point with the distant correction in place. When ametropia is fully Ordinary types used in printing are utilized for the correction of near vision (Fig. The patient is asked to hold the test-types carried out by asking the patient to read letters at a distance at which he is accustomed to read or over the colored panels on the vision drum. If the red letters are clearer than the green in myopia, it is certain that over-correction has not been done. But if the patient sees green letters more distinctly than the red, the patient is over-corrected. In all conditions where the visual acuity does not improve with the optical correction, a pin-hole disk test should be performed. However, no improvement in the visual acuity even with the pin-hole disk indicates some N 6 organic lesion in the macula. When I was ten years old, my father had a small estate near Satara where he used to take us during the holidays. It was situated in rough and uncultivated countryside where wild animals were often seen. Once we heard that there was a panther in the surroundings who was killing the cattle and attacking the villagers. The dog which helped Ramu ran barking at the hooves of the cows, who sometimes made a playful rush at the dog. They can be dyed correction so that the types are easily and comfortto reduce the transmission of light and surface ably read. Now the near point should be detercoated to check glare (anti-reflective coating). This is done by gradually bringing lenses should be securely fitted in light, strong towards the eye a card on which is drawn a line and rigid frames.
Parenchymatous division can be also accomplished by an ultrasonic surgical aspirator or by a high velocity water jet dissector anxiety 19th century buy luvox 100 mg without prescription. It is our opinion that in cirrhotic livers anxiety symptoms 9 days buy 50 mg luvox free shipping, transection is better achieved by Kelly crushing anxiety symptoms stomach best purchase luvox. Moreover anxiety symptoms kids buy luvox 50 mg online, an ultrasonic dissector is very useful in the isolation of portal branches anxiety disorder 3000 order 50 mg luvox, but is potentially harmful when used in the proximity of hepatic veins anxiety symptoms returning buy luvox pills in toronto. A device known as the harmonic scalpel (Ultracision) has been introduced on the market. The slowness during dissection, poor ergonomy and its cost have so far limited the use of this tool. At the end of liver transection, if this has been carefully conducted, oozing from the liver remnant is minimal. Sources of bleeding are identified, and haemostasis is achieved by absorbable mattress sutures on the raw surface. Careful inspection with a clean swab usually facilitates location of the origin of bile leakage. To improve further the haemostasis of the cut surface, fibrinogen sealant, microcrystalline collagen powder and argon beam coagulation have all been proposed. However, in our view careful haemostasis and securing of bile ducts during parenchymal transection is the best guarantee against postoperative collection and bile leakage. Abdominal drainage There is now strong evidence that abdominal drainage can be avoided even after hepatic resection. Partial or complete resection of the dorsal sector, which some years Resection of smal hepatocellular carcinoma in cirrhosis 105 ago was considered a hazardous operation, is technically feasible. It is worth mentioning that parenchymal transection during segmental resection causes more bleeding than during conventional hepatectomy, since there is no previous control of the portal pedicles and the raw surface following sectioning is large. There is an almost avascular plane, with the exception of one artery directed upwards to the liver that has to be ligated. Parenchymal division is shifted slightly to the left, thus preserving the middle hepatic vein. Note the location of the portal pedicle of segment V and the proximity of the tip of the right liver from the right area of resection. The latter is located higher in the parenchyma and should not be searched for at the hilus because of its depth. It is worth pointing out that there are no clear guiding landmarks for dividing between these two territories. Resection of smal hepatocellular carcinoma in cirrhosis 107 Segmentectomy V the limits of segment V are as follows: the main portal scissura on the left and the right portal scissura on the right, which is in the vicinity of the anterior tip of the right liver and the plane of the hilus posteriorly. After cholecystectomy, the main portal scissura is first opened up to the hilum, avoiding injury to the middle hepatic vein. Liver division is slightly displaced to the left in order to preserve the right hepatic vein. This manoeuvre facilitates the division of the posterior boundary of segment V, which has a transverse direction and is located at the level of the plane of the hilum. The main biliovascular pedicle of segment V is divided at the left superior corner of the resected specimen (Fig. After complete mobilization of the right liver, parenchymatous division is performed posteriorly and transversely at the level of the hilum without damaging the right hepatic Figure 5. The right portal scissura is opened on the right side of the right hepatic vein, which marks the anterior limit of the resection. Complete mobilization of the right liver up to the inferior vena cava and the distal portion of the right hepatic vein is paramount. The right portal scissura is then opened and divided in the direction of the inferior vena cava. Parenchymatous division is carried out, 1 cm to the right of the main portal scissura, taking care to ligate a large branch of the middle hepatic vein in the cranial portion of the liver division. The main pitfalls of this resection are injuries to the hepatic veins on the borders of the segment. Resection of smal hepatocellular carcinoma in cirrhosis 109 the portal pedicle is ligated intraparenchymally, taking care to avoid the accidental injury to the adjacent Figure 5. Removal of small tumours located in the left portion of the dorsal sector (segment I) is relatively easy to accomplish after liberation of segment I posteriorly from its connections to the vena cava, by sectioning the accessory veins and, anteriorly, by dividing the arterial and portal vein branches (Fig. However, similar to what has been suggested in a normal liver, 91, 92 procedures of isolated dorsal sectorectomy have been described also in cirrhosis. In the first, the liver is completely mobilized on both sides up to the insertion of the three main hepatic veins into the inferior vena cava by sectioning the right and left liver ligaments and dividing the accessory hepatic veins (Fig. The dorsal sector is freed from the inferior vena cava posteriorly and from the hilum anteriorly. The posterior branches of the portal vein directed to the dorsal sector are ligated and divided. Because of uncertainty as to the right border of the sector, Japanese authors have suggested injecting dye into the posterior portal branches. The resection starts from the Surgical management of hepatobiliary and pancreatic disorders 110 Figure 5. Note (A) the planes of dissection behind the portal vein and in front of the inferior vena cava and (B) the site of ligation of the accessory hepatic veins and posterior portal vein branches. In the second technique, dorsal sectorectomy can be performed by using a transhepatic approach, as described by Yamamoto et al. The liver is completely freed and transection is carried out along the main portal scissura, thus exposing the middle hepatic vein on most of its length. Pulling the resected dorsal sector forwards through the main portal scissura, the resection is ended by division of the portal branches directed towards the dorsal sector. The volume of non-tumourous liver removed is conspicuous (about 30%) and, therefore, the risks of hepatic failure and worsening portal hypertension are high. Moreover, the raw cut surface is the largest of the different hepatic resections and, as a consequence, postoperative fluid collection is not uncommon. Falciform and coronary ligaments are divided up to the inferior vena cava, whose anterior surface is exposed in order to locate the confluence of the hepatic veins, particularly the middle one, into the vena cava. It is actually harmful, in most cases, to encircle the pedicle: it is easier and safer to ligate it intraparenchymally during transection. If, for any reason, the right hepatic vein is encountered, the plane of section should be shifted medially. In front of the inferior vena cava, the trunk of the middle hepatic vein is easily identified and ligated on a vascular clamp by a running suture. Perioperative treatment Antibiotics Although some authors argue for the use of antibiotic therapy in cirrhotic patients undergoing liver resection, we do not routinely use this approach. Septic complications seem to be no higher in our patients compared to other series. In patients in whom a prolonged total portal clamping is foreseen, a preoperative selective intestinal decontamination may be proposed to prevent bacterial translocation. Blood transfusion the risks entailed in allogeneic blood transfusion are manifest in cirrhotic patients undergoing liver resection, and include worsening of hepatic function, increase in postoperative complications and a higher recurrence rate. Therefore all attempts should be made to identify patients at risk of bleeding in order to minimize the risk of transfusion. As shown in a multivariate study, 77 patients undergoing extended resections or with abnormal coagulation should be specially considered for other procedures, such as autologous blood predeposit, isovolemic haemodilution or intraoperative autotransfusion. While the procedure is mandatory in patients with benign tumours, its use in patients with malignant disease is debatable in view of the very high cost/benefit ratio. The best candidates for this procedure are those patients with Surgical management of hepatobiliary and pancreatic disorders 114 haemoglobin concentrations >13 g/dl. When haemoglobin is <11 g/dl, human recombinant erythropoietin and iron may also be effective in cirrhotic patients to accelerate erythrogenesis. Isovolemic haemodilution represents a very inexpensive and reliable method to substitute allogeneic transfusion in cirrhotic patients, 97 provided that contraindications such as major coagulation defects, cardiac disease or anaemia do not co-exist. Haemodilution is probably the best alternative method to allogeneic blood transfusion. The cell-saver for intraoperative blood recovery is practically unused in elective hepatic resection for malignant tumours because of its costs and the potential risk of tumoural cell dissemination, despite experimental evidence showing that this latter risk is absent. A policy of fluid and sodium restriction in cirrhotic patients is the best method for preventing ascites formation in the postoperative period. In the case of ascites formation, the intravenous administration of albumin or macromolecules associated with furosemide usually induces a diuresis and a reduction in intraperitoneal fluid accumulation. Paracentesis is mandatory in patients with massive ascites, in order to avoid prolonged leakage of fluid through the abdominal incision. Postoperative nutritional support is not a common practice after hepatectomy in our experience. Provided that a good selection of patients has been made preoperatively on the basis of residual hepatic function, the appearance of encephalopathy is nearly always exceptional. As a consequence, the use of special formulations, such as branched-chain amino acid enriched solution, does not lead to any clinical advantage over other standard formulations. An early resumption of oral intake in patients without complications is, in our current view, the best way to manage cirrhotic patients. When data from a number of series are collected, the mean 3and 5-year survivals are 59. In a large series of 1000 patients treated by hepatectomy Resection of smal hepatocellular carcinoma in cirrhosis 115 Table 5. Nevertheless, it must be mentioned that reinfection of the transplanted liver by hepatitis B or hepatitis C virus is the rule in cases of viral infection prior to transplantation, which might interfere with the risk of tumour recurrence. The high tumour recurrence rate after liver transplantation in this indication has prompted surgeons progressively to abandon liver transplantation for huge tumours. As regards the operative protocol, a thorough examination of the peritoneal cavity should be carried out before transplantation, and specific operative measures should be respected during the procedure. However, an alternative therapeutic approach which reduces the operative risk is right hepatectomy, preceded by an embolization of the right branch of the portal vein, provided that a compensatory hypertrophy of the left liver with an atrophy of the right liver has been achieved. This last result is most likely related to a more stringent selection Surgical management of hepatobiliary and pancreatic disorders 118 of patients for liver transplantation. Experience of 1000 patients who underwent hepatectomy for small hepatocellular carcinoma. Liver resection versus transplantation for hepatocellular carcinoma in cirrhotic patients. Adverse effects of preoperative hepatic artery chemoembolization for resectable hepatocellular carcinoma: a retrospective comparison of 138 liver resections. Morphological and histological features of resected hepatocellular carcinoma in cirrhotic patients in the west. Natural history of minute hepatocellular carcinoma smaller than three centimeters complicating cirrhosis. Natural history of small untreated hepatocellular carcinoma in cirrhosis: a multivariate analysis of prognostic factors of tumor growth rate and patient survival. Natural history of untreated non-surgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Prospective study of screening for hepatocellular carcinoma in Caucasian patients with cirrhosis. A multivariate analysis of risk factors for hepatocellular carcinogenesis: a prospective observation of 795 patients with viral and alcoholic cirrhosis. Concurrent hepatitis B and C virus infection and risk of hepatocellular carcinoma in cirrhosis. Risk factors for recurring hepatocellular carcinoma differ according to infected hepatitis virus. Elevations in serum alpha-fetoprotein levels in patients with chronic hepatitis B. Surgical management of hepatobiliary and pancreatic disorders 120 Early detection of primary hepatocellular carcinoma. Screening for primary hepatocellular carcinoma among persons infected with hepatitis B virus. Fine-needle aspiration biopsy of portal vein thrombus: value in detecting malignant thrombosis. Liver cancer imaging: the need for accurate detection of intrahepatic disease spread. Needle track seeding of primary and secondary liver carcinoma after percutaneous liver biopsy. Intrahepatic recurrence after resection of hepatocellular carcinoma complicating cirrhosis. Proposal of invasiveness score to predict recurrence and survival after curative hepatic resection for hepatocellular carcinoma. Patterns of recurrence after initial treatment in patients with small hepatocellular carcinoma. Chromosomal changes and clonality relationship between primary and recurrent hepatocellular carcinomas. Resection of smal hepatocellular carcinoma in cirrhosis 121 Analysis of 144 cases. Incidence and factors associated with intrahepatic recurrence following resection of hepatocellular carcinoma.