Penegra
Simon Dexter DM FRCS(Gen) FCSHK
- Consultant upper GI surgeon
- St James? University Hospital, Leeds, UK
Decompression is typically performed through a transconjunctival incision with a lateral canthotomy and inferior cantholysis prostate cancer treatment buy 100mg penegra amex, but a subciliary approach is used as well prostate cancer genetic testing order 100 mg penegra overnight delivery. The medial wall and orbital floor decompressions are of the most benefit in compressive optic neuropathy but have a slightly higher rate of diplopia post operatively prostate cancer fighting foods order penegra 50 mg with mastercard. The decompression is called "balanced" when the medial wall and lateral wall are included androgen hormone killing buy penegra 100mg overnight delivery. Studies have shown that the balanced decompression has lower rates of diplopia as compared to decompressions involving the floor prostate cancer 70 year old male order generic penegra on-line. Insights into the pathogenesis of thyroid-associated orbitopathy: evolving rationale for therapy prostate zonal anatomy mri order penegra paypal. Orbital fibroblast heterogeneity may determine the clinical presentation of thyroid-associated ophthalmopathy. Biologic therapeutics in thyroid-associated ophthalmopathy: translating disease mechanism into therapy. Reliability of estimating ductions in thyroid eye disease: an International Thyroid Eye Disease Society multicenter study. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Impact of smoking on the response to treatment of thyroid associated ophthalmopathy. Efficacy of Tocilizumab in Patients With Moderate-to-Severe Corticosteroid-Resistant Graves Orbitopathy: A Randomized Clinical Trial. Adalimumab as steroid-sparing treatment of inflammatory-stage thyroid eye disease. Infliximab: a novel treatment for sight-threatening thyroid associated ophthalmopathy. Teprotumumab, an insulin-like growth factor-1 receptor antagonist antibody, in the treatment of active thyroid eye disease: a focus on proptosis. Reduced risk of compressive optic neuropathy using orbital radiotherapy in patients with active thyroid eye disease. Normalization of upper eyelid height and contour after bony decompression in thyroid-related ophthalmopathy: a digital image analysis. Comparison of two different surgical techniques for the treatment of strabismus in dysthyroid ophthalmopathy. Change in proptosis following extraocular muscle surgery: effects of muscle recession in thyroid-associated orbitopathy. Methods: this review provides an update on current and emerging therapeutic options for retinoblastoma. The medical literature was searched for articles relevant to the management of retinoblastoma. The results of prospective and retrospective studies on chemotherapy and focal therapy for retinoblastoma are summarized. Results: Treatment strategies for retinoblastoma involve intravenous chemoreduction, local administration routes of chemotherapy (eg, intra-arterial, intravitreal), focal therapy for tumor consolidation (eg, photocoagulation, thermotherapy, cryotherapy, plaque brachytherapy), external beam radiotherapy, and surgical enucleation. Emerging therapies include alternative chemotherapeutic agents, molecularly targeted therapies, and novel drug-delivery systems. Conclusion: In the past 10 years, the management strategy for retinoblastoma has signifcantly changed, shifting toward local chemotherapy and away from systemic chemotherapy. Innovations in the feld of molecular biology and the development of targeted therapies have led to improvements in survival rates and ocular salvage for this disease. However, the need still exists to further assess the long-term effects of such directional changes in therapy. Major advances, such as our understand Retinoblastoma is the most common primary intraoc ing of the molecular biology of the tumor and the de ular malignancy in children; its incidence rate is 1 in velopment of targeted therapy, have improved survival 14,000 to 20,000 livebirths. In the United States, the3 other pediatric malignancies, retinoblastoma is rare, 5-year overall survival rate is 97%. With early diagnosis and aggressive, multi-5 modal treatment strategies, near-complete cure rates are possible, and many patients retain functional vi From the Department of Ophthalmology, Emory University School of Medicine, Atlanta, Georgia. The delivery increases exposure to intra Adjuvant therapy priorities in management are (1) pre ocular target areas, reduces overall venting metastasis, (2) reducing the Metastatic retinoblastoma systemic exposure and harmful late risk of long-term secondary tumors Intra-arterial effects, and improves effectiveness (eg, osteosarcoma, soft-tissue sarco and rates of tolerability. The intro Intravitreal ma), (3) saving the eye, and (4) pre duction of intra-arterial and intravit Periocular serving vision. Despite the lack of clinical and size of tumors within the eye, presence of vit trials, rates of survival and ocular preservation have reous seeding, age and health of the child, and the improved. In general, in 100% of group A eyes, 93% of group B eyes, 90% of unilateral tumors can be managed with focal therapy group C eyes, and 48% group D eyes. If genetic 2006); however, with the advent of local routes of ad testing is not performed, then patients with unilateral ministration (intra-arterial and intravitreal), use of sys disease require close follow-up of the unaffected eye temic chemotherapy has decreased in recent years. Alternatively, treat Intravenous chemotherapy is indicated as initial ment for bilateral tumors will depend on the extent of therapy for bilateral advanced disease in which at tumor in each eye. Chemo massive choroidal invasion, or any combination of op reduction is then usually followed by consolidation, tic nerve and choroidal invasion. Focal therapy may be employed as or hybrid regimens, typically delivered monthly for the only or initial therapy for small retinoblastoma 6 to 9 months. Surgical removal of Systemic chemotherapy for retinoblastoma is generally the eye or enucleation is reserved for very advanced safe and effective, but it is not without adverse events, (group E) cases. Treatment fail Management ure in the form of persistent vitreous seeds, subretinal Chemotherapy seeds, and intraretinal tumors following therapy have Intravenous: Systemic chemotherapy generally in been attributed to the inability of the treatment drugs volves a combination 2-, 3-, or 4-drug regimen deliv to reach the tumor. The most common Intra-Arterial: In the late 1980s, melphalan was ly used regimen is vincristine/etoposide/carboplatin. Vinca alkaloids such as vincristine bind tubulin dimers and block mitotic spindle formation. Reported adverse events include and carboplatin compromise the ocular vasculature transient vitreous hemorrhage, chorioretinal atrophy, in nonhuman primates and induces inflammation and extraocular tumor spread. Although it caused no systemic tox microemboli to the retina and choroid, myositis, icity in humans or rabbits, melphalan did result in sig eyelid edema, orbital congestion with resulting dys nifcant retinal toxicity at high doses and lower but safer motility, choroidal atrophy, optic atrophy, ophthalmic doses only achieved incomplete tumor control. Either carboplatin or ing to reduced surveillance and the undertreatment of topotecan can be employed. Subtenon chemotherapy us subretinal and vitreous seeds of tumor unresponsive ing carboplatin can increase tumor control, especially to laser treatment, conventional chemoreduction ther if it is coupled with intravenous chemoreduction. Another single therapy, but long-term follow-up revealed a high route of administration developed to address this prob failure rate as initial treatment; therefore, it should be lem is the intravitreal method, which involves injecting combined with other therapeutic approaches. The tumor may be ob in 51% of eyes after 10 years of follow-up; no cases served while on chemoreduction and, if unresponsive, of extraocular extension were reported during that foveal-sparing thermotherapy may be administered. Bilateral cases with small, extrafoveal tumors compared with 35% of those observed without consoli can be managed with focal treatments alone. Surgery6 treatment is typically performed within 24 hours of involves careful removal of the eye with minimal globe the intravenous chemotherapy cycle. Small posterior trauma to prevent tumor seeding into the orbit, and tumors without seeding respond well to laser photo then excising a long section of optic nerve for proper coagulation. In such cases, some form of chemother enough volume and allow the 4 rectus muscles to at apy can be used to shrink the tumor prior to the start tach for motility. Photocoagulation is also tissue should be harvested on a separate tray for ge used to treat tumor-associated retinal neovasculariza netic studies. Complications include vitreous seeding if the la A corollary to enucleation is the adequate histo ser power is too high, and retinal fbrosis, traction, and pathological evaluation of globe pathology, because vascular occlusion. An and < 2-mm thickness) tumors anteriorly located to the analysis of 1,020 study patients with high-risk features equator of the globe. Complications of cryotherapy in after enucleation showed that 24% of study volunteers clude retinal tears and detachment, proliferative vitreo at high risk developed metastasis if not treated with ad retinopathy, and chorioretinal atrophy. Because retinoblastoma has a high rate of proliferat External Beam Radiotherapy ing cells, it is quite radiosensitive. It is known to cause midfacial hypoplasia in ma, ocular brachytherapy is commonly used for uveal young patients and increase the risk of development of melanoma, in which a clinician uses a similar surgi soft-tissue sarcomas, brain tumors, osteosarcomas, and cal technique of plaque application of suturing to the other cancers. Animal models remain7 ography, computed tomography, and external beam) instrumental in understanding biological mechanisms should be avoided in individuals with heritable retino and designing targeted therapies for this disease. Treatment of orbital retinoblastoma includes single agent or in combination with other agents for systemic chemotherapy and external beam radiother the treatment of retinoblastoma. Most recurrences occur in the central of topotecan in fbrin sealant in humans have been nervous system and are associated with a low cure shown to achieve retinoblastoma tumor volume re rate; regimens proven to be effective include vincris duction. Craniospinal irradiation using 25 to noblastoma, topotecan avoids the retinal toxicity of 35 Gy is sometimes provided. Retinoblastoma may also melphalan, the nephrotoxicity of carboplatin, and the hematogenously spread to the bone marrow, bones, hematotoxicity of etoposide. For metastatic disease, multiple-agent, candidate drug for intravitreal injection because it has high-dose chemotherapy and autologous hematopoi minimal retinal toxicity and achieves maximum con etic stem cell transplantation can be administered as centration levels 50 times higher than systemic expo rescue therapy. The anthracycline idarubicin has seeds, causes minimal complications, and can achieve been shown to be effective against retinoblastoma tu a sustained treatment effect to retinoblastoma without mor cells in bone marrow (response rate, 60%), but spreading tumor cells. A sustained treatment effect is suffcient concentrations have not been achieved at desired because, even when compounds do reach the target sites (eg, central nervous system). Despite this lack8 cloned, yet no effective, molecularly targeted cure cur of clinical trials, rates of patient survival and ocular rently exists for retinoblastoma. Studies have shown that nutlin-3 restores Nanotechnology-based drug-delivery systems for the the p53 pathway in retinoblastoma cells lacking both treatment of cancer have signifcantly evolved during retinoblastoma protein and p53 activity, thus inducing the past decade by enabling options for site-specifc p53-mediated apoptosis. Cells lacking retinoblastoma protein near-infrared light, which enables the photothermal have increased E2F1 activity, and retinoblastoma-de destruction of cancer cells. Our laboratory is in intravitreal injection of gold-tethered liposomes and vestigating the suprachoroidal and intravitreal injec viral-like nanoparticles containing topotecan is being tion of topotecan using microneedles in a rabbit mod investigated in a rabbit model of retinoblastoma that el of retinoblastoma 2). Therapeutic op their bioactivity against retinoblastoma cells in cul tions for retinoblastoma have rapidly evolved in recent ture. Carboplatin released from a fbrin depot was also years, with a paradigm shift in standard treatment pro shown to decrease tumor burden in a transgenic mu tocols toward the targeted delivery of chemotherapeu rine model of retinoblastoma cells. Increased use of intra-arterial and intravit fbrin sealants sustained delivery of carboplatin in ocu real types of chemotherapy with focal consolidation, lar tissues compared with carboplatin in plain solution, along with the reduced use of systemic chemotherapy, which clears rapidly in vivo. However, these approaches are not Suprachoroidal Injection without complications, and a need still exists to weigh Suprachoroidal injection with microneedles is a route the risks and benefts of treatment and to evaluate their of targeted drug delivery to the choroid and retina that long-term effects. New therapies being investigated in poses minimal risk of extraocular tumoral spread, be clude novel carriers and routes for local drug delivery cause the vitreous and subretinal spaces are not en as well as molecularly targeted therapies. In a rabbit model, beva cizumab was determined to be safe and effective when injected A B into the suprachoroidal space; high concentrations were found in the posterior segment tis sues. When the mi croneedle injects compounds into the supraciliary space, these C D compounds posteriorly spread into the suprachoroidal space. Intra-arterial chemo therapy for retinoblastoma in 70 eyes: outcomes based on the international classification of retinoblastoma. Intra-arterial chemotherapy (ophthalmic artery chemosurgery) for group D retinoblastoma. Metastatic and non burden and economic cost: impact of age at diagnosis and selection of metastatic models of retinoblastoma. Update on intra-arterial chemo management: when to use intravenous, intra-arterial, periocular, and intra therapy for retinoblastoma. Retinoblastoma management: advances in for eyes severely affected by retinoblastoma masks risk of tumor extension enucleation, intravenous chemoreduction, and intra-arterial chemotherapy. Intraocular retinoblastoma: the case for a new real injections for retinoblastoma using an anti-reflux procedure and sterili group classification. Evaluating the risk of extraocular tumour pineal gland cyst and pineoblastoma in children with retinoblastoma during spread following intravitreal injection therapy for retinoblastoma: a system the chemoreduction era. Curr Treat Options for vitreous seeding in retinoblastoma: Recent advances and perspec Neurol. Retinoblastoma: direct chemotherapeutic bined chemotherapy and radiotherapy for advanced intraocular retinoblas drug delivery into the vitreous cavity. Transscleral drug delivery for posterior adjuvant chemotherapy for unilateral retinoblastoma following enucle segment disease. Retinoblastoma patients systemic versus focal Carboplatin chemotherapy in the rabbit eye: possible with high risk ocular pathological features: who needs adjuvant therapy Proceedings of the consensus hibitors in cancer, neurological diseases and immune disorders. Nat Rev meetings from the International Retinoblastoma Staging Working Group on Drug Discov.
Maternal urine toxicology screening was positive for cocaine and tetrahydrocannabinol mens health 2pm penegra 50 mg sale. The maternal use of opiates (eg prostate cancer calculator cheap 100mg penegra with amex, heroin mens health february 2014 generic 50mg penegra visa, methadone prostate 80cc generic penegra 100mg online, and buprenorphine) during pregnancy may be associated with withdrawal in the newborn prostate x-ray purchase 100mg penegra with visa. Affected newborns may present with symptoms at birth or up to 10 to 14 days later mens health 30 day six pack plan generic penegra 50mg amex. Maternal history and drug testing may be used to identify at-risk newborns, but it is important to note that synthetic opioids such as methadone are not detected on many routine urine toxicology screens. Many drugs used by mothers during pregnancy cross the placenta and affect the developing fetus, including agents associated with substance abuse. The potential effects of these agents include congenital malformations, prematurity, low birthweight, abnormal state regulation, and neonatal withdrawal (Item C203B). The severity of barbiturate withdrawal is similar to that seen with opioids, and typically presents 4 to 7 days after birth. The symptoms of alcohol and methamphetamine withdrawal are much less severe than those of opiate withdrawal. Although no specific treatments exist for nonopioid withdrawal in infants, clinicians must consider polysubstance exposure in newborns born to substance abusing mothers. The physical examination findings of excoriations, tachypnea, increased tone, and moderate tremors seen in the newborn in the vignette 3 days after delivery suggest opioid withdrawal. Methamphetamine and alcohol withdrawal are less likely, as they typically occur shortly after delivery. Although the urine toxicology screen of the mother in the vignette was positive for cocaine and tetrahydrocannabinol, these agents are not typically associated with the classic findings of neonatal abstinence syndrome. The repair requires sedation because of the boys age, anxiety level, and proximity of the laceration to the eye. Upon verbal stimulation, the boy opens his eyes, mumbles a few words, and falls back asleep. Moderate sedation is often required for laceration repairs in children from toddler to early school age, because of anxiety as well as pain. According to the American Academy of Pediatrics, moderate sedation is a state of decreased level of consciousness with appropriate response to physical stimulation or verbal commands. Monitoring should include continuous pulse oximetry, visual assessment of ventilation, and noninvasive blood pressure measurement every 5 minutes. For the boy in the vignette, the intended effect was not achieved after 1 dose of midazolam, as evidenced by continued screaming and thrashing, therefore a second dose was given. Adverse effects of benzodiazepines can include hypotension, bradycardia, and respiratory depression. The following equation can be used to estimate minimum systolic blood pressure for a young child: Systolic blood pressure = 70 mm Hg + (2 childs age in years)the child in the vignette has a systolic blood pressure of 68 mm Hg, which qualifies him as hypotensive. However, because he is not profoundly hypotensive, there is no indication of significant overdose, and he has adequate clinical perfusion, the boy is not likely on the verge of cardiovascular collapse. An important mechanism of hypotension caused by benzodiazepines is dilation of systemic arterioles and venules. The resulting increase in vascular capacitance can decrease preload, thereby reducing cardiac output. Administration of a fluid bolus will increase preload and therefore cardiac output, thereby increasing the blood pressure. Atropine is not recommended in this case because the child does not have bradycardia. Although epinephrine would increase blood pressure by causing vasoconstriction and increase cardiac output by its inotropic properties, it should be reserved for more profound shock states. Flumazenil is a reversal agent for benzodiazepines, but is not routinely recommended because of rebound effects and a risk of seizures. Naloxone is an opioid reversal agent, and would not be helpful in benzodiazepine overdose. Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: addendum. Her exposures include 2 dogs and 2 birds at home and consumption of unpasteurized cheese from Mexico. Imported unpasteurized dairy products, especially from Mexico, are a large source of Brucella infection in the United States. Transmission can also occur by inoculation of infected animal fluids into cuts, mucous membranes, or through inhalation. The diagnosis of Brucella is made by isolating the organism in culture or obtaining Brucella-specific serology. Children are estimated to account for up to one-third of all cases of brucellosis in endemic countries, although underreporting is possible. Common clinical manifestations of brucellosis include fever, sweating, osteoarticular complaints, hepatosplenomegaly, and transaminitis. Adults are more likely to have involvement of other sites, including the sacroiliac joint or axial skeleton. Bone marrow suppression can occur, as evidenced by the mild leukopenia observed in this patient. Brucella is an intracellular pathogen that can evade immune responses, therefore prolonged (minimum of 6 weeks) combination antimicrobial therapy is needed for effective treatment and to prevent relapses. While abdominal ultrasonography may show enlargement of the liver and spleen, this would not be a specific finding. Abdominal ultrasonography could be helpful in the diagnosis of hepatosplenic cat scratch disease caused by Bartonella henselae, where microabscesses may be visualized. However, this patient does not have feline exposure, making this a much less likely possibility. Chest radiograph can additionally help identify hilar lymphadenopathy and chest masses. However, this patient lacks respiratory complaints or pulmonary findings on physical examination, making pneumonia less likely. Additionally, given her exposure history, Epstein-Barr virus infection is less likely. Lastly, the negative urinalysis makes the likelihood of urinary tract infection, diagnosed with urine culture, low. Her physical examination is significant for a medium to large-sized vulvar hematoma with superficial abrasions (Item Q206). In children presenting with history of injury to the perineum, it is important to differentiate between accidental and nonaccidental (sexual abuse) trauma. A detailed history and physical examination is warranted in all cases of children with genital trauma. The extent of perineal injury on examination should correlate with the history to confirm nonsexual trauma as the cause of the patients injury. Caregivers of patients with accidental genital trauma generally seek immediate medical attention. The verbal child can give a supportive history of the accident and there may be witnesses (other family members) to the event. Physical examination in the presence of a chaperone should be performed in a patient with a history of perineal injury. In premenarcheal girls, the genital examination is best performed in the supine (frog leg) and the prone (knee chest) position. The prone (knee chest) examination is indicated in cases with suspected vaginal trauma. The examination may be difficult in a patient with a recent history of trauma and pain from the trauma. In these cases, local anesthesia (application of 2% lidocaine) or procedural sedation (such as in patients requiring sutures) is indicated. Vulvar hematomas and superficial lacerations (vulvar and vaginal) are the usual straddle injuries in girls. The vulvar area in young girls is highly vascular, with loose subcutaneous tissues increasing the risk for large hematoma formation. Therefore, complaints of bleeding or blood stains on the underwear are common in patients with straddle injuries and vulvar hematomas. Urinary retention may be associated with vulvar hematomas and the physician needs to ensure proper voiding before discharging the patient home. Patients with large hematomas and urinary retention may need temporary bladder drainage. Most hematomas are usually managed conservatively with adequate pain control, rest, ice packs, and tub baths. Patients are advised to rest on their side or use a foam or air-filled rubber doughnut (while sitting) to avoid pressure injury of the swollen external genitalia. Surgical intervention may be needed in patients with injury to the pelvic floor, urethra, or increasing hematoma size despite adequate conservative management. Straddle injuries may lead to unilateral and superficial lacerations of the vagina and vulva. The patient in the vignette has lacerations in the right hymenal wall and fourchette. Identification of vaginal lacerations from accidental trauma is important, as penetrating injuries (from sexual abuse) are usually associated with vaginal lacerations in children. Bleeding from hymenal injuries is often minimal and usually requires no treatment. Complaints to adults or caregivers of uncomfortable experiences from being touched on the genitalia, inappropriate sexualized behaviors (excessive masturbation, adult words associated with sexuality, simulation of sexual behavior with siblings or toys), symptoms of vaginal discharge, genital lesions suggestive of sexually transmitted disease, and genital or anal injuries on physical examination are suspicious for underlying sexual abuse. In patients, U or V-shaped clefts (notches) of the posterior rim (from 3 oclock to 9 oclock), indicative of healing after a laceration and attenuation or decreased width (less than 1 mm) of the posterior hymen, are suggestive for underlying sexual abuse. It is important to note that only a small percentage of sexually abused children have an abnormal genital or anal finding. Clinicians should also be aware of the age-related hymenal changes and normal anatomic variations of the hymen, which may be confused with features of sexual abuse. Midline sparing (linea vestibularis), developmental variants (fenestrated hymen, failure of midline fusion), labial adhesions, and dermatologic conditions such as lichen sclerosus and pemphigoid may be confused with features of sexual abuse. For the patient in the vignette, the presenting history, symptoms (of blood in the underwear), and physical examination (vulvar hematoma and acute superficial lacerations) are consistent with straddle injury. She has a 3-month history of worsening right upper quadrant abdominal pain and bloody diarrhea. The next step in evaluation of this child is to refer for colonoscopy to obtain tissue for diagnosis. The differential diagnosis of gastrointestinal bleeding varies by age and origin of the bleeding (Item C207). A complete history and physical examination follows stabilization and should include visualization of a stool sample. Stool cultures and Clostridium difficile toxin should be completed to evaluate for infectious etiologies. Tagged red blood cell scans and angiography can be used, but are not effective at localization if the rate of blood loss is low, as is typical in children. He was a full term spontaneous vaginal delivery without complications during pregnancy or delivery. Initial development was normal for the first few months, which then slowed compared to his peers. The neurologic examination reveals dystonia, spasticity, extensor plantar reflexes, and increased deep tendon reflexes. Therefore, the best next test to aid in the patients clinical diagnosis would be a urinary urate-to-creatinine ratio. At birth, patients appear normal, but by 3 to 6 months of age, hypotonia and developmental delay become evident. In the first several years, unusual motor movements manifest, including dystonia, choreoathetosis, and opisthotonos. Spasticity, hyperreflexia, and extensor plantar reflexes that mimic cerebral palsy also become apparent. The behavioral disturbances and cognitive decline emerge between 2 and 3 years of age. A pathognomonic clinical finding of Lesch-Nyhan disorder is self-injurious behaviors, as seen in the child in this vignette. Uric acid overproduction leads to deposition of uric acid crystals in the bladder, kidneys, and ureters over time. The index of suspicion is raised when developmental delay is concurrently seen with hyperuricemia or nephrolithiasis. The urinary urate-to-creatinine ratio, the best screening test, should be greater than 2. Diagnostic confirmation is made via analysis of the hypoxanthine-guanine phosphoribosyltransferase enzyme activity, which should be less than 1. Therefore, males who carry the gene change are affected, but females are carriers and are typically unaffected. Treatment is directed at controlling the uric acid production with allopurinol for the urate nephropathy, gouty arthritis, tophi, and nephrolithiasis; however, this treatment has no impact on the behavioral and neurologic symptoms of the disorder. Patients typically require therapies, including habilitative, behavioral, and psychiatric therapy.
Discount penegra on line. CREAMY BLACK BEAN QUINOA SALAD | VEGAN HEALTHY LUNCH OPTION.
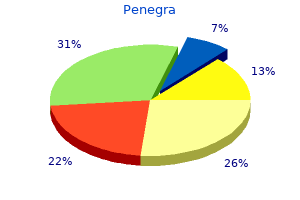
Less than monthly referring to key words in the questions: cut down; annoyed; C prostate cancer awareness month purchase penegra 50 mg online. Nutritional In men prostate-7 review cheap 100mg penegra with mastercard, a total score of 4 or more points is a positive indicator of deficiencies and unhealthy habits can cause or contribute to oral patients at risk for hazardous drinking or alcohol use disorders mens health 60 years old penegra 50 mg mastercard. Dentists can play an important role in educating patients on the importance of good nutrition to oral and systemic health man health nursing environment cheap penegra online. Like tobacco androgen receptors in hormone-dependent and castration-resistant prostate cancer buy 50 mg penegra mastercard, alcohol can be carcinogenic to humans prostate 800 order penegra in united states online, and heavy Dr Zenchenko is a second-year resident, Department of Family use is a major risk factor for the development of both precan Medicine, Tripler Army Medical Center. Long term treatment with metformin in patients with type a synergistic effect on each other. As with tobacco use, the 2 diabetes and risk of vitamin B-12 deficiency: randomised placebo controlled trial. By providing 7 kcal/g, it decreases the appetite, associated with levodopa-carbidopa intestinal infusion: a long-term prospective assessment. Nutrition for oral health and oral manifestations of poor nutrition and unhealthy habits 6. Fruit juice in infants, children, and adolescents: current recommen servicestaskforce. Folic acid supplements and risk of facial clefts: national org/en/about-the-ada/ada-positions-policies-and-statements/statement-on-early population based case-control study. The incisor teeth of albino rats and guinea pigs in vitamin A deficien mic control in people with diabetes mellitus. Correlative clinico-pathological evaluation enamel in 2 to 6-year-old Saudi boys. Smoking tobacco, oral snuff, and alcohol in the etiolo Academy of Pediatrics Committee on Nutrition. Prevention of rickets and vitamin D deficien gy of squamous cell carcinoma of the head and neck: a population-based case-referent study cy in infants, children, and adolescents. Final Recommendation Statement: Tobacco Smoking vitamin D metabolites in postmenopausal osteoporosis. Mineral balance and bone turnover in adolescents RecommendationStatementFinal/tobacco-use-in-adults-and-pregnant-women-counseling with anorexia nervosa. Screening and counseling for unhealthy alcohol use in primary care tobacco smoking, and cancer. Guidelines Related to Alcohol, Nicotine, and/or Drug Use by dent effects of alcohol drinking and tobacco smoking on oral cancer: a large case-control Child or Adolescent Patients. Statement on Alcohol and Other Substance Use by Pregnant International Head and Neck Cancer Epidemiology Consortium. While much of this may already be familiar, the way one approaches a patient with a neuro ophthalmic problem differs somewhat from the approach used in general ophthalmology and the examination techniques are often unfamiliar to general ophthalmologist and neurologists. Neuro-ophthalmic deficits may involve complex neuro-anatomic pathways, and the differential diagnosis may be (or appear to be) quite broad. Once a lesion has been localized to a particular neurologic or ophthalmologic structure, one is in a far better position to generate an appropriate differential, and decide what further work-up (if any) is required. For example, the diagnostic evaluation for a patient with a lesion localizing to the retrochiasmal visual pathways would be quite different than that for a patient with retinal or optic nerve disease. Some people find it easier to think of each neuro-ophthalmology patient as a puzzle. Although each may differ in the degree of complexity, no puzzle makes sense until all the pieces fit together appropriately. A careful history is a critical piece of the puzzle, and the neuro-ophthalmic examination should function as the natural extension of the history. If you begin the examination with some idea as to where in the visual system the problem resides, it becomes easier to focus on pertinent positive and negative findings. As a general rule of thumb, if the history doesnt match the exam, one of them (or both! Afferent Pathway Symptoms 3 Nature of visual symptoms When confronting a patient with visual loss, it is important to identify the specific type of visual loss the patient is describing. Try to nail down whether the patient is actually describing decreased visual acuity (poor clarity of images), or complete loss of vision, localized visual field loss, scotoma, etc. Diplopia and oscillopsia (subjective sense that objects are moving) may be reported by patients as blurred vision, but have separate differential diagnoses. It is also critical to determine if the visual symptoms are monocular or binocular. Monocular visual loss suggests that the lesion is anterior to the optic chiasm. In practice, patients are sometimes unable to distinguish whether one eye or both eyes are involved: since the temporal visual field is larger than the nasal, patients with homonymous visual field defects often localize vision loss to the eye with the temporal field cut. For example, a patient describing unilateral waviness and distortion of central vision (metamorphopsia) almost certainly has a macular lesion, and the rest of the history and exam can be used to confirm that diagnosis. Onset and duration of visual lossthe onset, duration, and tempo of visual loss provide valuable clues as to etiology, and may also determine the urgency of further evaluation. Sudden loss of vision most commonly results from a vascular or inflammatory process, whereas slowly progressive visual loss suggests a compressive, toxic/nutritional, or infiltrative process. The presence or absence of pain should be specifically addressed, since this will often distinguish vascular (painless) from inflammatory (painful) etiologies. It is very uncommon in the 60s, rare in the 50s, and unheard of under the age of 50. In patients with transient episodes of visual loss, the first question again is whether it involved one or both eyes. Visual loss from a transient ischemic event typically lasts 3-5 minutes, while the transient visual obscurations seen with papilledema generally last for seconds. Ask about photopsias visual phenomena such as flashing lights, scintillations, flashing black squares and distortions in vision such as metamorphopsia or micropsia. These phenomena may be associated with retinal disease, migraines, and epileptic seizures. Make sure to ask about symptoms associated with the visual loss, especially if these symptoms occurred at the time of the episode. Pertinent symptoms would include weakness or numbness on one side of the body, slurred speech, difficulty swallowing, word-finding problems, and imbalance. Certain retinal dystrophies may be associated with hemeralopia (day blindness) or nyctalopia (night blindness); it is often helpful to ask the patient whether they prefer to see in dim or bright light. Its worth remembering that difficulty at night is a common symptom for many ophthalmic diseases, including cataract and refractive error patients with true nyctalopia have profound dysfunction in dim environments, and often need to be led around or refrain from driving. Efferent Pathway Symptoms Diplopia may result from a large variety of disorders, and localization, both by history and examination, is particularly important. Monocular diplopia, except in rare circumstances, is the result of an ocular abnormality, such as refractive error or tear film insufficiency. If the diplopia is binocular, the patient should be asked if the diplopia is horizontal, vertical, or oblique; if it is particularly worse or better in one direction of gaze; and if it is different when viewing at distance or near. For example, the history of horizontal binocular diplopia, worse at distance and worse on 5 left gaze immediately implicates the left lateral rectus as the weak muscle and allows you to perform the rest of the history and exam in a much more focused fashion. As a general rule, the goal of evaluating the efferent pathway is to localize to one (or more) of the following locations: Supra-nuclear (cortical and sub-cortical) rd th th Nuclear and inter-nuclear (3, 4, 6 nerve nuclei and medial longitudinal fasciculus) rd th th Nerve (3, 4, 6) Neuro-muscular junction (myasthenia gravis, botulism, etc) Extra-ocular muscle (thyroid eye disease, orbital myositis, etc) You should ask about previous episodes of diplopia, or a history of childhood strabismus or head tilt. Many patients with a previously well-controlled phoria will decompensate later in life or after even minor head trauma. Some clues to this diagnosis include: full versions; concomitant deviation; prior history of patching or strabismus surgery; and impaired sensory testing with evidence of suppression (stereoacuity, Worth 4 dot, etc). Ask the patient if the diplopia is constant or intermittent, and if intermittent, if there is a pattern to when it occurs. For example, in myasthenia gravis, symptoms are typically absent or minimal in the morning, and worsen throughout the day, whereas with thyroid eye disease, symptoms are worse in the morning, and improve throughout the day. Always ask about any associated ptosis or pupillary abnormalities, as this may suggest the involvement of one or more cranial nerves. It is important to ask about associated neurologic symptoms such as bulbar weakness (dysarthria, dysphagia) and proximal muscle weakness (difficulty arising from a chair, climbing stairs, brushing hair). These symptoms may be associated with myasthenia as well as certain hereditary and acquired neuromuscular diseases. Patients with vestibular imbalance often complain of disequilibrium or unsteadiness. Oscillopsia is an illusory to-and-fro movement of the environment that may be horizontal, vertical, torsional, or a combination of these directions. These symptoms most commonly reflect a mismatch among vestibular, visual, and somatosensory inputs concerning the position or motion of the body in space. The chief concern in such patients is to identify, 6 by history and examination, whether the vestibular dysfunction is central (brainstem/cerebellum) or peripheral (labyrinth, vestibular nerve). Patients with central vestibular imbalance, in addition to having impaired eye movements (saccades and smooth pursuit) and central vestibular nystagmus (in most but not all cases) may report ataxia, dysarthria, dysphagia, facial numbness or weakness, or diplopia. Such symptoms, with corroborating physical findings, mandate neuroimaging and further investigation. Most cases of peripheral vestibular imbalance are benign and self-limited, and do not necessarily require neuroimaging or extensive investigations. Additional Medical Historythe patients medical history often provides useful information. Patients with hypertension and diabetes mellitus are more predisposed toward ischemic events than those without such risk factors. Medications, surgeries, and previous traumatic injuries may all be relevant to the presenting complaint. Any history of malignancy also deserves special attention, particularly if it is a malignancy known to metastasize to brain (breast, lung, renal cell, etc). Another general rule of thumb: a new neuro ophthalmic deficit in a patient with a known (and recent) history of cancer should be attributed to either the cancer or its treatments until proven otherwise. It is important to remember that the medical diagnosis that the patient self-reports should not be considered securely diagnosed without adequate documentation or verification. For example, if a patient reports a history of stroke, lupus, etc, a few follow-up questions should be asked to determine whether the diagnosis is secure. This is particularly important when the presenting complaints may be related to the self-reported diagnosis. A more detailed discussion of these examination techniques may be found in standard Ophthalmology and Neurology texts. Visual Acuity and Refraction Both distance and near visual acuity should be tested. A discrepancy between distance and near acuity may be due to several factors, including media opacities and accommodative insufficiency. Further, functional patients may not understand the relationship between near and distance visual acuity, and may provide inconsistent responses. A good refraction, or even the use of the pinhole, can correct optical abnormalities resulting in loss of vision, and therefore prevent an expensive and time consuming workup. Patients may have significant loss of visual function even with relatively preserved visual acuity. Color Vision Color vision testing is the secret weapon of the neuro-ophthalmologist, and often helps differentiate neurogenic from non-neurogenic visual loss. With mild optic nerve dysfunction, impaired color perception may be present when visual acuity is only minimally affected. Acquired dyschromatopsia may be seen with lesions of the optic nerve, retina, or the visual cortex. It should be noted that cerebral dyschromatopsia, typically caused by lesions at the occipital-temporal lobe junction, is rarely isolated, and often accompanied by other focal neurologic symptoms, including homonymous visual field defects. The control plate (the first plate) does not assess color vision, but tests whether visual acuity is good enough to proceed with the rest of the test. For example, a patient with a dense cataract may have normal optic nerve function, but not be able to read the control plate due to poor visual acuity from media opacity. When color plates are unavailable, a difference in color perception between the two eyes may be identified using a colored bottle top. All of the visual field techniques (including automated perimetry and Goldmann kinetic perimetry) are prone to error both patient related and technician related. Ask if any parts of the face are missing; small central scotomas may be identified using this method. Have the patient compare the examiners eyes and upper and lower face for differences; altitudinal defects may be readily detected by this method. This latter technique will usually only pick up absolute scotomas, typically homonymous defects, since the target size is so large. Since 90% of the primary visual cortex subserves macular vision (central 30), checking exclusively for large peripheral defects is often unproductive. Since red wavelengths are lost first when the visual pathways have been damaged, a small red target may detect relative visual field defects, particularly central scotomas. Formal perimetry is far more sensitive than confrontation field testing, and is required if a visual field defect is suspected. This usually manifests as severe constriction, which is itself non-specific but can reflects optic nerve, retinal, or visual cortex pathology. However, it is insufficient to simply demonstrate that the visual field 10 loss has a functional component, since this gives no information about the true status of the visual system a significant number of patients have combined organic and functional vision loss. One method is to do finger-to-nose perimetry: have the patient look at your face and then touch your fingers in the periphery, telling them that you are testing coordination (which is technically true). If they can accurately identify and touch your finger in all 4 quadrants, that proves normal or nearly normal field. Even if they dont respond, they may make accurate saccades to the target in each quadrant, which also indicates normal or at least better than claimed visual field.
Conservative treatment with special eyeglasses may be suffi cient even in irreversible cases prostate cancer 50 year old male penegra 50mg for sale. Because of the risk of overcorrecting or undercorrecting the disorder prostate cancer exam age order penegra 100mg fast delivery, several operations may be necessary mens health ipad order penegra 50 mg visa. Prognosis and complications: Prompt surgical intervention in congenital ptosis can prevent amblyopia mens health 9 minute kettlebell workout effective penegra 100mg. Surgical overcorrection of the ptosis can lead to desiccation of the conjunctiva and cornea with ulceration as a result of incomplete closure of the eyelids prostate cancer pathophysiology buy penegra with amex. The margin of the eyelid and eyelashes or even the outer skin of the eyelid are in contact with the globe instead of only the conjunctiva prostate cancer young order 50 mg penegra otc. The following forms are differ entiated according to their origin (see Etiology): O Congenital entropion. Epidemiology: Congenital entropion occurs frequently among Asians but is rare among people of European descent, in whom the spastic and cicatricial forms are more commonly encountered (see also Chap. Etiology: O Congenital entropion: this results from fleshy thickening of the skin and orbicularis oculi muscle near the margin of the eyelid. The frontalis suspen sion technique may employ autogenous fascia lata or plastic suture. O Cicatricial entropion: this form of entropion is frequently the result of postinfectious or post-traumatic tarsal contracture (such as trachoma; burns and chemical injuries). Causes can also include allergic and toxic reactions (pemphigus, Stevens-Johnson syndrome, and Lyells syndrome). Symptoms and diagnostic considerations (see also etiology): Constant rubbing of the eyelashes against the eyeball (trichiasis) represents a per manent foreign-body irritation of the conjunctiva which causes a blepharo spasm (p. Treatment: O Congenital entropion: To the extent that any treatment is required, it con sists of measured, semicircular resection of skin and orbicularis oculi muscle tissue that can be supplemented by everting sutures where indi cated. O Spastic entropion: Surgical management must be tailored to the specific situation. Usually treatment combines several techniques such as shorten ing the eyelid horizontally combined with weakening or diverting the pre tarsal fibers of the orbicularis oculi muscle and shortening the skin verti cally. O Cicatricial entropion:the surgical management of this form is identical to that of spastic entropion. An adhesive bandage may be applied to increase tension on the eyelid for temporary relief of symptoms prior to surgery. Prognosis and complications: Congenital entropion is usually asymptomatic and often resolves within the first few months of life. O Spastic entropion:the prognosis is favorable with prompt surgical inter vention, although the disorder may recur. Left untreated, spastic entropion entails a risk of damage to the corneal epithelium with superin fection which may progress to the complete clinical syndrome of a serpigi nous corneal ulcer (see p. O Cicatricial entropion:the prognosis is favorable with prompt surgical intervention. The following forms are differentiated according to their origin (see also Etiology): O Congenital ectropion. Epidemiology: Senile ectropion is the most prevalent form; the paralytic and cicatricial forms occur less frequently. Congenital ectropion is very rare and is usually associated with other developmental anomalies of the eyelid and face such as Franceschettis syndrome. O Senile ectropion:the palpebral ligaments and tarsus may become lax with age, causing the tarsus to sag outward. O Paralytic ectropion: this is caused by facial paralysis with resulting loss of function of the orbicularis oculi muscle that closes the eyelid. O Cicatricial ectropion: Like cicatricial entropion, this form is usually a sequela of infection or injury. At the same time, the ever sion of the punctum causes tears to flow down across the cheek instead of draining into the nose. A proven procedure is to tighten the lower eyelid via a tarsal wedge resection followed by horizontal tightening of the skin. O Paralytic ectropion: Depending on the severity of the disorder, artificial tear solutions, eyeglasses with an anatomic lateral protective feature, or a watch glass bandage. In severe or irreversible cases, the lagophthalmos is treated surgically via a lateral tarsorrhaphy. O Cicatricial ectropion: Plastic surgery is often required to correct the eyelid deformity. The deformity causes the eyelashes to run against the con junctiva and cornea, causing a permanent foreign-body sensation, increased tear secretion, and chronic conjunctivitis. The disorder may also be successfully treated by cryo cautery epilation or surgical removal of the follicle bed. Etiology: In addition to photosensitivity and increased tear production, blepharospasm will also accompany inflammation or irritation of the anterior chamber. Symptoms: Clinical symptoms include spasmodically narrowed or closed palpebral fissures and lowered eyebrows. Severe cases may require transection of the fibers of the facial nerve supplying the orbicularis oculi muscle. The disorder may also be successfully treated with repeated local injections of botulinum toxin. Cosmetics, adhesive bandages, or eyedrops and eye ointments are often responsible, particularly the preservatives used in them such as benzalkonium chloride. They cause typical reddening, swelling, and lichenifica tion of the skin of the eyelid. Symptoms: Reddening, swelling, lichenification, and severe itching of the skin of the eyelid occur initially, followed by scaling of the indurated skin with a sensation of tension. Etiology:the skin of the eyelid is affected intensively by infectious and aller gic processes. For example, it may be more intense in the early morn ing after the patient rises than in the evening. The constitution of the skin, seborrhea, refractive anomalies, hypersecretion of the eyelid glands, and external stimuli such as dust, smoke, and dry air in air-conditioned rooms often contribute to persistent chronic inflammation. Symptoms and diagnostic considerations:the margins of the eyelids usu ally exhibit slight inflammatory changes such as thickening. The eyelashes adhere due to the increased secretion from the glands of the eyelids, and scaly deposits form. The scales and crusts can usually be softened with warm olive oil and then easily removed with a cotton-tipped applicator. Prognosis:the prognosis is good although the clinical course of the disorder is often quite protracted. Etiology: Infection of the skin of the eyelids results when latent herpes sim plex viruses present in the tissue are activated by ultraviolet radiation. The virus spreads along sensory nerve fibers from the trigeminal ganglion to the surface of the skin. Symptoms: Typical clustered eruptions of painful vesicles filled with serous fluid frequently occur at the junction of mucous membranes and skin. The patient should avoid intense ultraviolet radiation as a prophylactic measure against recur rence. Epidemiology:the disorder usually affects immunocompromised persons between the ages of 40 and 60 who have underlying disorders. Etiology:the disorder is caused by the varicella-zoster virus, which initially manifests itself as chickenpox. If activation or reinfection occurs, the latent neurotropic viruses present in the body can lead to the clinical syndrome of herpes zoster ophthalmicus. Prodro mal symptoms of erythema, swelling, photosensitivity, and lacrimation may occur before the characteristic clear watery vesicles appear. The skin sensitivity at the tip of the nose should be evaluated on both sides in the initial stage of the disorder. Decreased sensitivity to touch suggests involvement of the nasociliary branch of the ophthalmic nerve, which can lead to severe intraocular inflammation. Complications: Involvement of the nasociliary branch of the ophthalmic nerve can lead to severe intraocular inflammation. Etiology: An abscess of the upper or lower eyelid can form as a sequela of minor trauma, insect sting, or spread of inflammation from the paranasal sinuses. Symptoms:the severe inflammation and swelling often make it impossible actively to open the eye. Orbital cellulitis or cavernous sinus thrombosis can occasionally occur as a sequela of eyelid abscess, especially when located at the medial angle of the eye. Application of a 2% mercury precipitate ointment over an extended period of time is also effective. Symptoms and diagnostic considerations: Hordeolum presents as painful nodules with a central core of pus. External hordeolum appears on the margin of the eyelid where the sweat glands are located. Internal horde olum of a sebaceous gland is usually only revealed by everting the eyelid and usually accompanied by a more severe reaction such as conjunctivitis or che mosis of the bulbar conjunctiva. Differential diagnosis: Chalazion (tender to palpation) and inflammation of the lacrimal glands (rarer and more painful). Treatment: Antibiotic ointments and application of dry heat (red heat lamp) will rapidly heal the lesion. An underlying inter nal disorder should be excluded in cases in which the disorder frequently recurs. Epidemiology and etiology: Chalazia occur relatively frequently and are caused by a chronic granulomatous inflammation due to buildup of secretion from the meibomian gland. After introducing the chalazion clamp, the lesion is incised either medi ally, perpendicular to the margin of the eyelid, or laterally, perpendicu lar to the margin of the eyelid (this is important to avoid cicatricial ectropion). A higher incidence has also been observed in patients with diabetes, increased levels of plasma lipoprotein, or bile duct disorders. The disease usually affects children and teenagers and is transmitted by direct contact. The pinhead-sized lesions have typical central depressions and are scattered near the upper and lower eyelids. The cutaneous horn should be surgically removed as 25% of keratosis cases can develop into malignant squamous cell carcinomas years later. Differential diagnosis should exclude a basal cell carcinoma (see that section); the margin of a keratoacanthoma is characteristically avascular. They frequently (25% of all cases) develop into a malignant squamous cell carcinoma in later years if they are not surgically removed. Symptoms: Hemangiomas include capillary or superficial, cavernous, and deep forms. Diagnostic considerations: Hemangiomas can be compressed, and the skin will then appear white. Differential diagnosis: Nevus flammeus: this is characterized by a sharply demarcated bluish red mark (port-wine stain) resulting from vascular expansion under the epidermis (not a growth or tumor). Treatment: A watch-and-wait approach is justified in light of the high rate of spontaneous remission (approximately 70%). Where there is increased risk of amblyopia due to the size of the lesion, cryotherapy, intralesional steroid injections, or radiation therapy can accelerate regression of the hemangioma. Neurofibromatosis is regarded as a phacomatosis (a developmental disorder involving the simultaneous presence of changes in the skin, central nervous system, and ectodermal portions of the eye). Symptoms and diagnostic considerations:the numerous tumors are soft, broad-based, or pediculate, and occur either in the skin or in subcutaneous tissue, usually in the vicinity of the upper eyelid. They can reach monstrous proportions and present as elephantiasis of the eyelids. Morbidity in sunny countries is 110 cases per 100000 persons (in central Europe approximately 20 per 100000 persons). Increased exposure to the suns ultraviolet radiation, carcinogenic substances (such as arsenic), and chronic skin damage can also lead to an increased inci dence. Basal cell carcinomas arise from the basal cell layers of the epidermis and the sebaceous gland hair follicles, where their growth locally destroys tissue. Symptoms: Typical characteristics include a firm, slightly raised margin (a halo resembling a string of beads) with a central crater and superficial vascular ization with an increased tendency to bleed. Ulceration with gnawing peripheral proliferation is occasionally referred to as an ulcus rodens; an ulcus terebans refers to deep infiltration with invasion of cartilage and bone. Diagnostic considerations:the diagnosis can very often be made on the basis of clinical evidence. Treatment:the lesion is treated by surgical excision within a margin of healthy tissue. Prognosis:the changes of successful treatment by surgical excision are very good. The firm, painless swelling is usually located in the upper eyelid and is mobile with respect to the skin but not with respect to the underlying tissue. An apparent chalazion that cannot be removed by the usual surgical procedure always suggests a suspected adenocarcinoma. Orbital part of the Superior punctum lacrimale lacrimal gland Superior lacrimal canaliculus Fundus of the lacrimal sac Plica semilunaris Lacrimal sac Nasolacrimal duct Inferior concha Inferior punctum lacrimale. A palpable lacrimal gland is usually a sign of a pathologic change such as dacryoadenitis. The tendon of the levator palpebrae muscle divides the lacrimal gland into a larger orbital part (two-thirds) and a smaller palpebral part (one-third).